Posted February 18, 2020 in Male Fertility Procedures
8 minute read
Getting pregnant can be more challenging than it seems, with recent studies suggesting that about 1 in every 5 women have difficulty conceiving
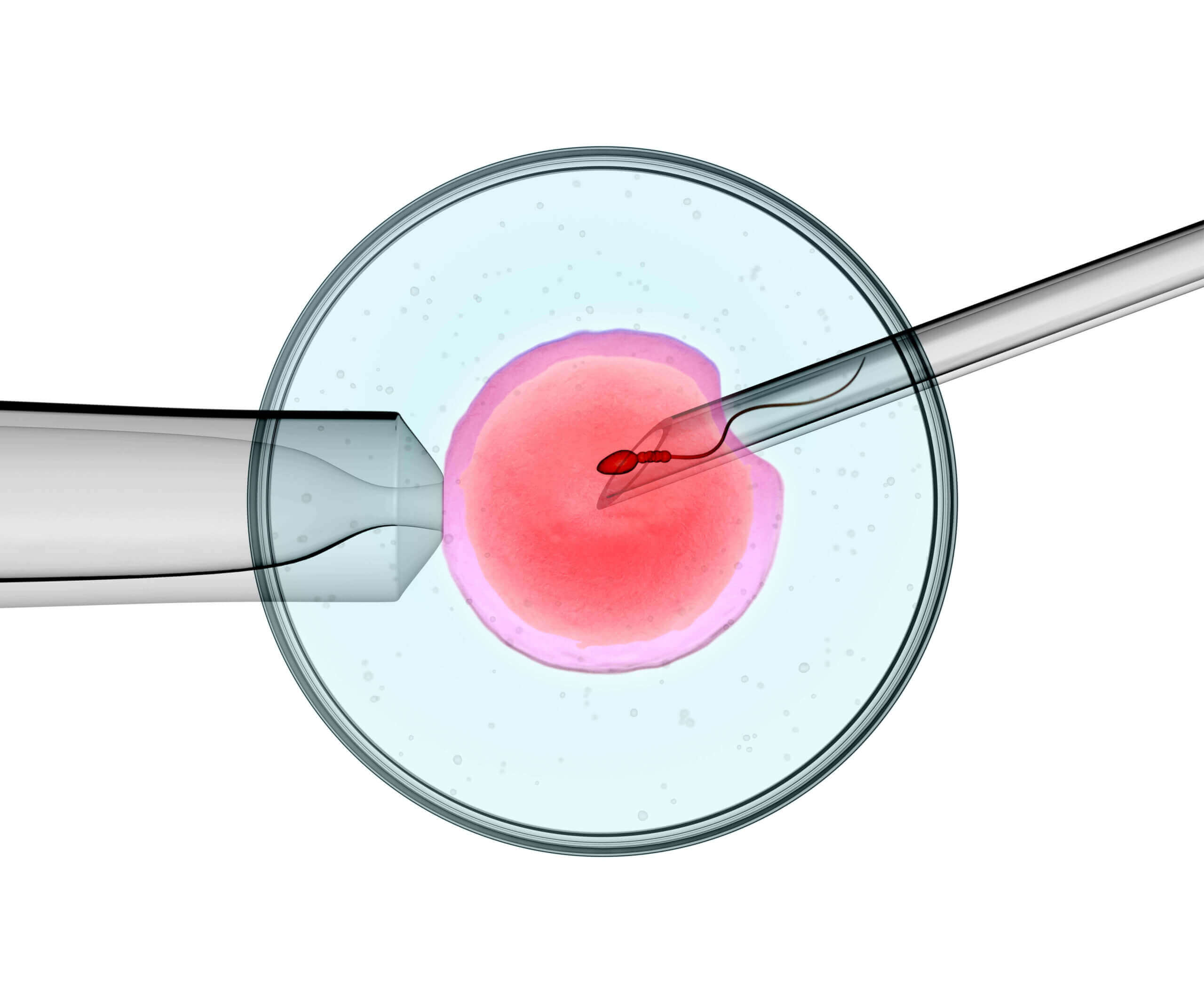
Before a sperm can fertilize an egg, the head of the sperm has to attach to the outer layer of the egg. It then pushes through the outer layer into the cytoplasm of the egg and moves towards its center where fertilization takes place. However, sometimes the sperm may fail to penetrate the egg’s outer layer for several reasons discussed below.
But there’s still hope for couples with who have trouble conceiving naturally or with intrauterine insemination – intracytoplasmic sperm injection (ICSI). This laboratory procedure involves the direct injection of a sperm cell into an egg outside the woman’s body.
Read on to learn more about the ICSI procedure.
Why is ICSI Performed?
There are several reasons for ICSI, including:
Low Sperm Count
Also known as oligospermia, low sperm count means that the semen ejaculated during intercourse contains fewer sperm cells than normal. When the semen contains zero sperm cells, the condition is known as azoospermia.
There a range of causes of low sperm count such as:
- Genetic Conditions
- Excessive alcohol and drug use
- Infections
- Varicocele
- Ejaculation problems
- Hormone imbalances
- Undescended testicles
- Frequent exposure to heat
If a man’s sperm count is less than 15 million sperms per milliliter of semen, it’s considered lower than average.
Low sperm counts significantly reduce the chances of a sperm cell fertilizing the egg and therefore lessens the chance of pregnancy. Fortunately, during ICSI sperm is directly injected into the eggs, increasing the odds of fertilization and pregnancy.
Abnormal Sperm Morphology
Sperm morphology is the shape and size of the sperm, and it’s one of the top factors used to evaluate fertility in men. Healthy sperm have oval heads with long tails. Abnormally shaped sperms have head and/or tail defects that reduce their effectiveness.
For example, a sperm cell may have a double or crooked tail or a misshapen head. These morphological defects affect the sperm’s ability to reach, penetrate, and fertilize the egg.
Low Sperm Motility
Sperm motility is the ability of sperm to swim efficiently to the egg. Good motility is a crucial factor in the fertilization process.
There are two main types of sperm motility – progressive motility and non-progressive motility.
Progressive motility means that the sperm are mostly moving in a straight line or large circles.
Non-progressive sperm motility, on the other hand, means that the sperm don’t swim in a straight line. For sperm to swim through the woman’s reproductive tract and fertilize the egg, it needs to have progressive motility of at least 25 micrometers per second.
Men whose semen analysis demonstrates a lot of non-progressively motile sperm have asthenozoospermia, the inability of the sperm to swim efficiently to the egg.
Unsuccessful IVF Procedures
In Vitro Fertilization (IVF) is an egg fertilization process where the egg is incubated with many sperm cells outside the woman’s body to allow fertilization to occur.
If a couple has had standard IVF procedures before and none of the eggs were fertilized, ICSI may be a viable option for them. ICSI is a procedure that is added to the IVF procedure so that sperm are injected into the eggs instead of just being placed next to the eggs.
Vasectomy Reversal Failure
For men who previously had a vasectomy but later changed their mind, vasectomy reversal is a cost-effective option to regain fertility. This procedure reconnects the vas deferens, tubes that carry sperm from the testicles to the man’s prostate where they enter the semen.
After the procedure, a man can get his partner pregnant. However, pregnancy rates after vasectomy reversal can be as low as 30 percent. If a couple is unable to get pregnant after a vasectomy reversal, surgically collected sperm (testicular or epididymal) can be harvested and directly injected into the egg for fertilization.
Blocked Tubes
Apart from a failed vasectomy reversal, the surgical collection of sperm may be necessary if there’s a blockage that prevents sperm from reaching the semen. This can be due to injury, disease, a genetic disorder (e.g. Cystic Fibrosis), or even an extremely low sperm count.
How is ICSI performed?
An intracytoplasmic injection is when the sperm gets injected into the cytoplasm of a mature egg with a tiny needle known as a micropipette. This helps eliminate the need for the sperm to penetrate the egg’s outer layer. ICSI is done as part of the IVF cycle.
Once fertilization takes place, the fertilized egg (embryo) grows in the IVF laboratory for about five days. It can be transferred into the woman’s uterus at that time or a later date if genetic tests are to be performed.
The ICSI technique was first used on human eggs in 1988. It was mostly used for cases where the standard IVF procedures failed. However, it was until 1992 when the first ICSI pregnancies succeeded.
ICSI’s capacity to permit almost all types of sperms to fertilize the egg has made it one of the most reliable treatments for male infertility.
How is the Egg Retrieved for ICSI?
The egg retrieval is a surgical procedure done under sedation. The ovarian follicles are aspirated using a tiny needle with the help of transvaginal ultrasonography.
A trained embryologist will scan the follicular fluids to find all the available eggs. The retrieved eggs are then stored and cultured in a specific IVF media in the lab until fertilization.
How is Sperm Retrieved for ICSI?
For men with low sperm motility and/or low sperm count, the collection of sperm cells can occur through normal ejaculation.
For cases where vasectomy reversal fails, needle aspiration or surgical sperm retrieval is an excellent alternative to surgery. This process allows physicians to get an adequate amount of sperm for the ICSI procedure, using a tiny needle that extracts sperm from the testicles. It’s performed under sedation with little to no discomfort.
ICSI vs. IVF vs. IUI: What’s the Difference?
ICSI is usually confused with IVF and IUI. However, these procedures are all different.
IUI (Intrauterine Insemination) is a procedure where sperm from the man is “washed” so that it can be safely placed in the female partner’s uterus. The “good” sperm then gets inserted into the uterus through the cervix with a catheter. This procedure is suitable for men with slightly low sperm counts or motility since the sperm doesn’t have to travel far to reach the egg. It’s also the least invasive of the three options.
In IVF (In Vitro Fertilization), the eggs are taken out of the woman’s body and are placed with motile sperm. Fertilization of the egg occurs naturally but in order to increase the odds of fertilization, a large amount of healthy sperm is required. Hence, this may not be the right choice for men with low sperm count. After fertilization, the fertilized egg (embryo) will be transferred into the woman’s uterus.
What is the Success Rate for ICSI?
The use of ICSI as a solution to male infertility in the U.S. has increased significantly since its inception.
In 2016, IVF with ICSI comprised more than 66 percent of all Assisted Reproductive Technology (ART) procedures. The ICSI procedure fertilizes a higher percentage of eggs than IVF alone. This can result in more embryos and increase a couple’s chance of conceiving by giving them more embryos to transfer, although many factors are involved in determining clinical pregnancy rates.
What are some of the Risks of ICSI IVF?
While the fertilization rates of IVF with ICSI may be high, not all fertilized eggs develop into healthy embryos. Factors such as the woman’s age, egg and sperm quality, and condition of the eggs all affect pregnancy rates. Birth defects associated with ICSI specifically are rare with a 1 percent chance of occurrence. Some of the defects that can occur with IVF and ICSI include sex chromosome abnormalities, Hypospadias, Angelman syndrome, and Beckwith-Wiedemann syndrome, and can be associated with the fact that male partner has fertility issues in the first place. For example, a male child conceived through ICSI may have the same infertility complications as their fathers. Compared to natural fertilization, there’s also a slight risk that ICSI may allow unhealthy sperm to fertilize the egg, potentially leading to an embryo that fails to develop.
Keep in mind that even with regular fertilization, there’s a 3-4 percent chance of birth defects which is similar to the general population that does not have fertility issues.
Another risk of IVF or IVF with ICSI is the increased chance of multiple or higher-order births (twins, triplets, or higher). Controlling the number of embryos that are transferred into the woman’s uterus can substantially lower this risk. Like naturally conceived children, children that are from twin or higher-order multiple pregnancies may be prone to birth defects or developmental problems. The goal of most good clinics is to transfer one or two high-quality embryos per attempt.
Final Thoughts on Intracytoplasmic Sperm Injection (ICSI)
Patients should understand the potential risks and complications of Intracytoplasmic Sperm Injection before the procedure is undertaken. It is essential to do your research and find an expert. At Inovi Fertility & Genetics Institute, we are committed to providing the best IVF, ICSI & Personalized care in the Houston fertility market.
