Posted January 26, 2025 in Fertility Blog & Information
12 minute read
Key Takeaways
- A septate uterus is the most common congenital uterine anomaly. It can have a profound effect on fertility, making education and awareness about the condition extremely important for all women of reproductive age.
- For women with a septate uterus, the fertility implications can be great. These challenges, such as implantation failure and increased rate of miscarriage, highlight the need for accurate diagnosis and management.
- Hysteroscopic septum resection is a definitive surgical treatment for a septate uterus. Correcting a septum can dramatically enhance reproductive outcomes and reduce the chance of experiencing complications during pregnancy.
- Women with a septate uterus should be counseled on non-surgical management. Making lifestyle changes and using fertility medications offer promising alternatives that can help them have the children they desire.
- Comprehensive management strategies, including pre-pregnancy planning and vigilant monitoring during pregnancy, are essential for managing potential complications and optimizing outcomes.
- Emotional and psychological support are integral to the process for women facing a septate uterus and the resulting fertility impact. Counseling and support networks give them the tools to process grief and rage, to adapt, to carry on.
A uterine septum is a type of congenital uterine anomaly where a fibrous band divides the uterus. This condition can affect fertility and increase the chance of having miscarriages. Understanding that a septum is present is key to having the conversation regarding fertility options.
While not everyone with a septum experiences complications, education and professional support can provide understanding and reassurance. Fortunately, treatment options—including surgical removal—are effective at helping women achieve live births.
This introduction provides a foundation for exploring the intricate relationship between uterine septum and fertility, ensuring informed decisions and personalized care. When people have the right information, they are better able to tackle their reproductive challenges with skill and conviction.
What Is a Septate Uterus
Definition and Anatomy
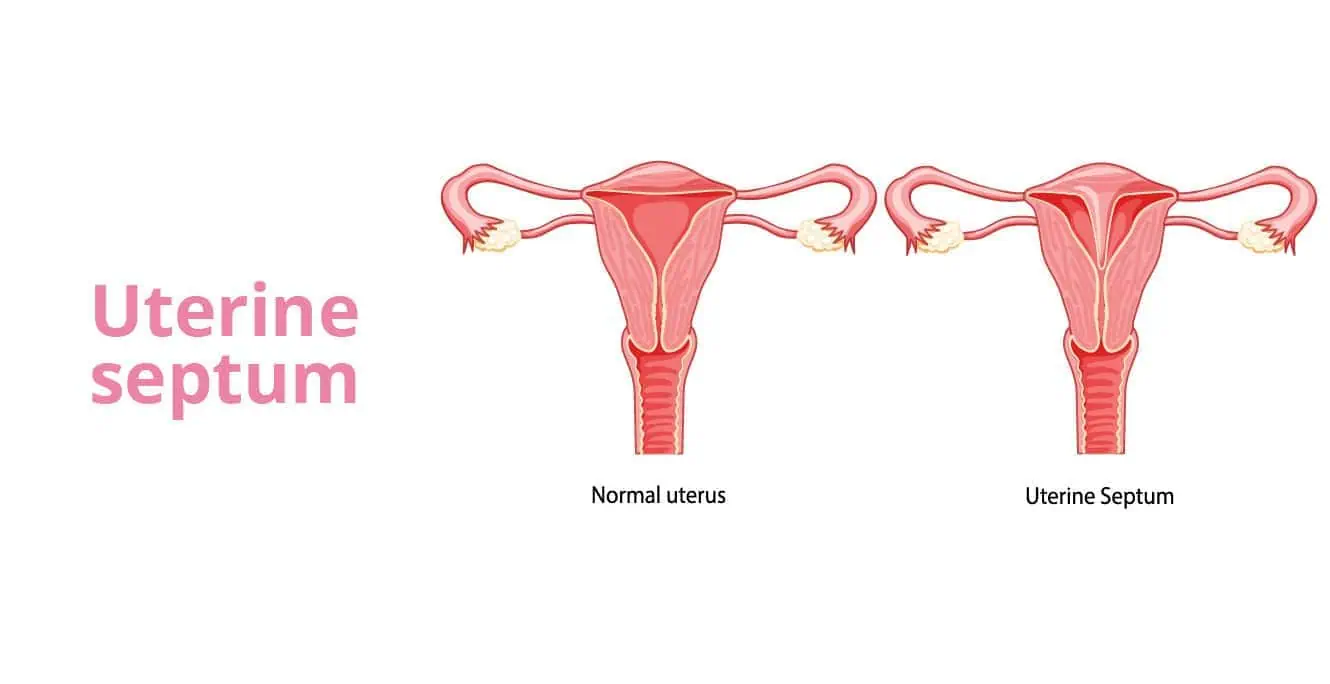
A septate uterus is a congenital anomaly in which a fibrous or muscular septum divides the uterine cavity. This septum creates a uterus that, instead of being shaped like an upside-down pear, is divided down the middle with a wall of tissue.
Whereas a typical uterus has one open cavity, a septate uterus has a septum that is partial or entirely divides the cavity in two. How a septate uterus differs from other anomalies is significant. For instance, a bicornuate uterus is heart-shaped, and a unicornuate uterus has just one horn.
Depending on the size and placement of the septum, it can affect how the uterus works. Our endometrium, or uterine lining, is very central to our reproductive health. It’s necessary for the process of implantation. A septum can interfere with this process, impacting both fertility and pregnancy outcomes.
Prevalence Among Women
The septate uterus represents approximately 35% among all uterine anomalies. In the general population, its prevalence is about 1% to 2%.
Though a septate uterus is uncommon, awareness is important, particularly among women of childbearing age. According to the statistics, 4% of the general population who have a uterus are living with this condition.
It’s associated with a 35% rate of miscarriage and complications such as preterm birth. Nonetheless, surgical techniques such as hysteroscopic metroplasty can increase the potential for pregnancy success.
Diagnostic techniques including 3D ultrasound assist in the accurate diagnosis of this anomaly, aiding in improved treatment choices.
Impact on Fertility and Pregnancy
1. Fertility Challenges
A septate uterus can pose fertility issues because of its effect on implantation and embryo growth. This results in a hostile environment for the embryo making it difficult for the embryo to implant properly, frequently resulting in implantation failure. The septum is a thin membrane of tissue that can make it difficult for an embryo to adhere.
This interference creates a hostile environment for the embryo, preventing it from successfully implanting in the uterine lining and developing. For individuals needing assisted reproductive technologies such as IVF, having a septate uterus only adds to the challenge of achieving a positive outcome. Women who opt for hysteroscopic metroplasty generally have more positive outcomes.
They experience a cumulative pregnancy rate of 71.0%, compared to only 59% for those who forgo the procedure.
2. Pregnancy Complications
Women with a septate uterus are at risk for multiple pregnancy complications, like abnormal fetal positioning and placental accreta. The presence of a septum may limit the room for fetal movement and cause the fetus to be breech or transverse.
It can lead to placental dysfunction, raising the risk of pregnancy complications. Ongoing surveillance is important to ensure that these risks are adequately addressed. Hysteroscopic metroplasty has been demonstrated to reduce these complications, enhancing live birth rates and overall pregnancy outcomes.
3. Miscarriage Risks
Evidence shows that an untreated septate uterus puts women at risk for miscarriage, with women frequently experiencing early and recurrent losses. The structural abnormality can make it impossible for the embryo to be adequately sustained, causing pregnancy loss.
Surgical intervention, such as hysteroscopic metroplasty, greatly decreases these risks. Thus far, this procedure has proven to be successful in improving conditions within the uterine cavity, increasing the rate of successful pregnancies, and reducing the frequency of miscarriages.
4. Preterm Birth Concerns
Pregnancies with a septate uterus have a higher risk of preterm birth. Uterine malformations may lead to complications such as cervical incompetence, increasing the risk of premature delivery.
Conservative management and timely intervention, such as surgical management, are essential in reducing these risks. Research shows that hysteroscopic metroplasty increases fertility results.
This innovative procedure markedly improves the overall structure and function of the uterus, helping even women with a long history of failed pregnancies.
Diagnosing a Septate Uterus
Diagnostic Tests
Identifying a uterine septum involves several diagnostic tests, each offering unique insights into reproductive outcomes.
- A special X-ray that uses a dye to highlight the uterine cavity and fallopian tubes, helping in spotting abnormalities.
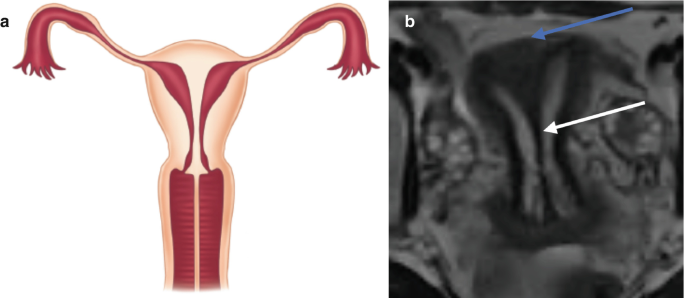
- This innovative technique gives us a comprehensive look at the outer uterine contour. Recommended as the first-line diagnostic tool, it’s noninvasive and can be augmented with saline infusion for greater diagnostic accuracy.
- Provides highly detailed images of soft tissues, useful for complicated cases requiring additional information.
- Hysteroscopy: Not only diagnostic but therapeutic, this procedure allows direct visualization and potential correction of the septum.
Imaging Techniques
Now side by side, we can see each imaging technique’s strengths as well as its weaknesses. Among these, three-dimensional ultrasound is unique because of its accuracy and noninvasiveness.
It is great at visualizing the uterine cavity and is more readily available than MRI. Hysteroscopy has two roles, both diagnosing and treating septate uterus, effectively restoring reproductive outcomes.
With an increased pregnancy success rate of around 65% after the procedure, it’s a critical option. Accurate diagnosis is important.
It informs which treatment route to pursue while addressing risks it poses, including miscarriages that happen at a higher rate in those with anomalies in their uterus.
Here is where gynecologists can make a tremendous difference, as their knowledge and experience in identifying symptoms can lead to vital, life-saving intervention.
Treatment Options for Septate Uterus
Understanding the available treatments for a uterine septum is essential for enhancing fertility and improving reproductive outcomes. Treatment options can be categorized into surgical and non-surgical methods, tailored to meet the unique needs and reproductive goals of each patient.
Surgical Interventions
One of the main surgical treatments is hysteroscopic septum resection. Because the procedure uses a hysteroscope to remove the septum, the procedure is minimally invasive. Bipolar technology is becoming more commonplace to help with this, providing additional safety and ensuring better outcomes.
In most cases, the success rate for achieving pregnancy after the procedure is 60-80%. Metroplasty, the other surgical alternative, attempts to reestablish normal uterine anatomy and function by excising the septum. Careful advanced surgical techniques are needed to prevent complications and guarantee the best outcomes.
For women who have major subseptations measuring greater than 1 cm, surgical repair is advised.
Non-Surgical Approaches
Non-surgical management may include lifestyle modifications and careful monitoring. Fertility medications can play a role in enhancing reproductive success for women opting out of surgery. Regular assessments and support are important to ensure patient well-being.
Advanced imaging techniques like 3D transvaginal ultrasound are key for accurate diagnosis and monitoring, providing a noninvasive first-line diagnostic tool.
Management Strategies
The key to dealing with a septate uterus, or any uterine abnormality, is an individualized, holistic approach focused on each woman’s unique needs. This begins with planning before conception, during which time it is imperative to consult with fertility specialists. They help navigate patients to required diagnostic testing, such as hysteroscopy, which has a 100% accuracy in identifying conditions like a complete septate uterus.
When surgery is indicated, most physicians still prefer hysteroscopic septoplasty. This procedure has a very low rate of complications at only 1.7%, with a 71% pregnancy success rate. It is important to raise the discussion of surgical options with the scissors versus resectoscope both demonstrating similar delivery rates. That’s why a personalized fertility plan is so important. It considers key factors, including the median time from surgery to pregnancy, which is about 5.5 months.
Even then, during the course of pregnancy, intense vigilance is essential to monitor and manage the risk of complications. Routine ultrasounds and fetal biophysical profiles are used to monitor fetal growth and the uterine environment. Continuous monitoring allows for a proactive approach to address concerns in a timely manner, especially for women with a history of recurrent miscarriage.
Our collaborative care team of gynecologists, fertility specialists, and mental health providers plays a crucial role in this process. Patient education plays an essential role as well. By allowing people to better understand their conditions and treatment options, it plays an important role in protecting the mental health of all people.
Additional Considerations
Psychological Impact
Coping with a septate uterus can take a serious toll on one’s emotional health, particularly when dealing with infertility or the loss of a pregnancy. This is an overwhelming and distressing thing to hear. After all, congenital anomalies such as this only affect roughly 4% of those with a uterus.
Not only is the emotional toll unmeasurable, there’s a greater chance of miscarriage. For women with a septate uterus, that risk increases to nearly 35%, whereas it is just 10% to 20% for other women. Luckily, if you’ve had surgery to fix this anomaly, you have an 80% chance of being able to carry a baby to term.
Making use of mental health resources can be a positive coping mechanism. Support networks are key to addressing these challenges in a comprehensive manner.
Support and Counseling
Creating a powerful support network is equally important for those facing recurrent miscarriages.
- Fertility support groups for shared experiences and advice.
- Counseling services to provide professional mental health support.
- Online forums and communities to facilitate 24/7 access to credible information and to each other.
- Educational workshops to better understand reproductive health.
Importance of Research and Awareness
Continued research should be the priority to ensure the best outcomes for women with uterine anomalies. With increased awareness, we can improve diagnosis and provide more effective treatment options.
Improving care through education is essential. Understanding the embryological origins of a septate uterus is critical for educating both medical and support communities.
Conclusion
Understanding the shape of a uterine septum allows for informed decisions regarding fertility to be made. Understanding what a septate uterus is and how it affects pregnancy can help you take the right next steps. Identifying it sooner gives patients and practitioners time to consider the most effective treatment options. Treatments such as surgery provide an avenue toward better fertility results. Effective management strategies make the trip a little smoother, providing resources and treatments that fit each person’s unique lifestyle. Making the decision to correct a septate uterus with professional medical guidance leads to improved preparation and care.
If you’re dealing with this condition, we encourage you to seek care from providers who are experts in reproductive health. They’re able to give individualized guidance and more targeted treatment plans. What’s most important is to be proactive. Keep in mind, knowledge is power when it comes to making informed health choices.
Frequently Asked Questions
What is a septate uterus?
A septate uterus, a common congenital uterine malformation, features a fibrous band of tissue that divides the uterine cavity, potentially leading to reproductive difficulties and adverse pregnancy outcomes.
How does a septate uterus affect fertility?
A septate uterus, a type of uterine abnormality, may raise the risk of recurrent miscarriage and fertility issues by preventing proper embryo implantation.
How is a septate uterus diagnosed?
Diagnosis of uterine abnormalities is made through imaging tests such as ultrasound or MRI, while hysteroscopy can confirm the presence of a uterine septum.
What are the treatment options for a septate uterus?
The primary treatment for uterine abnormalities is surgical removal of the septum, known as hysteroscopic metroplasty, which greatly increases reproductive outcomes.
Can a septate uterus be managed without surgery?
In others, surgical intervention like uterine septum resection is necessary to repair the uterine abnormality. Always consult your healthcare provider for advice tailored to your circumstances.
Are there any risks associated with surgery?
Increased surgical risks such as infection, bleeding, and uterine perforation can affect obstetrical outcomes; however, with skilled surgeons, results are mostly favorable.
What should I consider before treatment?
Consider your fertility goals, risks, and recovery time, especially if you have a history of recurrent miscarriages or uterine abnormalities. Discuss your options with a healthcare professional to ensure the best reproductive outcome for your situation.
