Posted December 09, 2024 in Fertility Blog & Information
17 minute read

The latest innovations in IVF technology are transforming dreams into reality for countless families on their fertility treatment journey, overcoming the insurmountable infertility challenge with quality fertility care and changing the way fertility treatments are approached. Breakthroughs in genetic screening, embryo selection, and cryopreservation are making treatments more effective and accessible. These advancements promise higher success rates and healthier pregnancies. New techniques like preimplantation genetic testing (PGT) allow for better embryo selection, reducing the risk of genetic disorders. Enhanced freezing methods ensure that embryos remain viable for future use. With these cutting-edge developments, patients can navigate their fertility journeys with renewed hope and confidence. Explore how these innovations are reshaping the landscape of reproductive health and offering new possibilities for those seeking to conceive.
Key Takeaways
- Stay informed about the latest IVF technologies to enhance your understanding and options for fertility treatments.
- Consider microfluidic technology, which improves embryo selection and can lead to higher success rates in IVF.
- Explore advances in fertility methods, as they can offer new solutions for individuals facing challenges in conception.
- Genetic testing innovations are crucial; they help identify viable embryos and reduce the risk of genetic disorders.
- Understand cryopreservation techniques, as they allow for better preservation of eggs and embryos for future use.
- Keep an eye on the role of deep learning in IVF, as it may revolutionize how fertility specialists analyze data and improve treatment outcomes.
Understanding IVF and Its Importance
Definition of IVF
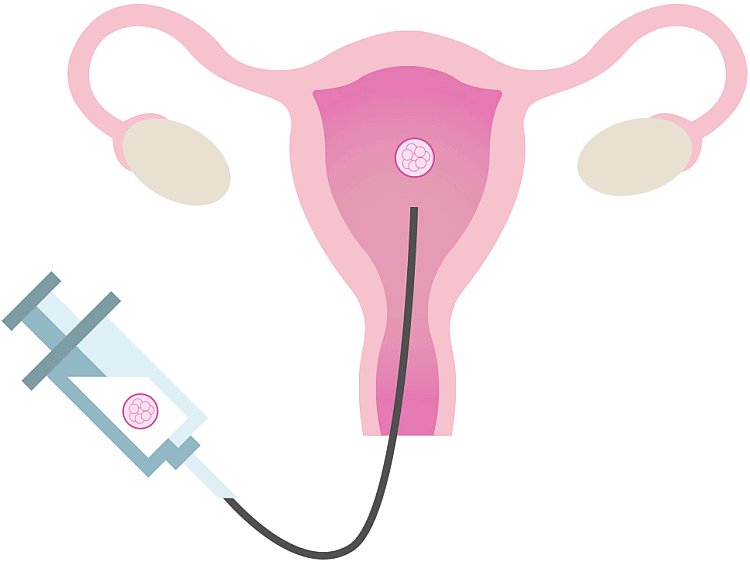
IVF stands for In Vitro Fertilization. This process helps individuals and couples who struggle with infertility. It involves combining eggs and sperm outside the body in a lab. Once fertilized, the embryos are placed back into the uterus. This procedure offers hope to many who wish to start or expand their families.
Emotional Impact
The journey through IVF can be emotionally challenging. Patients often experience a mix of excitement and anxiety. Each step can bring hope, but it also carries the fear of failure. Many feel overwhelmed by the medical procedures and hormonal treatments involved.
Families may also face stress during this time. Partners must support each other while managing their emotions. The need for open communication is crucial. Couples often find comfort in sharing their experiences with others facing similar challenges.
Psychological Effects
The psychological effects of IVF can be profound. Anxiety and depression are common among patients. The pressure to succeed can weigh heavily on them. Many worry about how they will handle setbacks if the treatment does not work.
Support groups play an important role in helping individuals cope. Sharing stories and feelings can lessen feelings of isolation. Professional counseling may also assist those struggling with emotional burdens.
Advancements in Research
Ongoing research is vital for improving IVF outcomes. Scientists continuously seek new methods to enhance success rates. For example, preimplantation genetic testing allows doctors to screen embryos for genetic conditions. This technology increases the chances of healthy pregnancies.
Another area of innovation is cryopreservation, or freezing eggs and embryos. This technique allows women to preserve their fertility for future use. It gives them more control over their reproductive choices.
Importance of Technology
Technological advancements have transformed IVF practices. Improved lab techniques lead to better embryo culture conditions. These innovations increase the likelihood of successful implantation.
Artificial intelligence is now being used in IVF clinics. AI algorithms help analyze embryo quality more accurately than ever before. This technology assists embryologists in making informed decisions about which embryos to transfer.
Recent Developments in IVF
Legislative Changes
Recent legislative changes have impacted modern IVF practices. In the United States, the Affordable Care Act (ACA) has improved access to fertility treatments. Many states now require insurance coverage for IVF. This change helps more IVF patients afford the necessary treatments.
In Europe, countries like the UK are also updating their regulations. The Human Fertilisation and Embryology Authority (HFEA) oversees IVF practices. They ensure safety and effectiveness in clinics. New guidelines focus on embryo viability rates. These rates help doctors select the best embryos for transfer.
Research Initiatives
Recent research initiatives aim to enhance clinical IVF methods. Studies show that preimplantation genetic testing (PGT) can improve success rates. PGT allows doctors to screen embryos for genetic disorders before implantation. This technology increases the chances of a healthy pregnancy.
Another area of research involves improving embryo culture conditions. Scientists study how different environments affect embryo development. Optimizing these conditions can lead to better outcomes for patients undergoing IVF.
Outdated Laws
Outdated laws can hinder progress in IVF technology and research opportunities. Many regulations were created years ago and do not reflect current scientific advancements. For example, some laws limit the number of embryos that can be created or stored. This restriction may prevent patients from accessing the best possible treatment options.
In some regions, laws surrounding embryo disposition remain unclear. Patients often face difficult choices about unused embryos. These outdated regulations can create emotional stress for those involved.
Advocacy Organizations
Organizations like the British Fertility Society play a crucial role in advocating for modernized IVF regulations. They work to promote evidence-based practices in fertility treatment. Their efforts include lobbying for policy changes that benefit IVF laboratories and patients alike.
The society also provides resources for healthcare professionals. This guidance helps them stay updated on the latest recent research and innovations in IVF technology. By supporting education and training, they ensure that practitioners offer the best care possible.
Microfluidic Technology Transformations
Device Revolution
Microfluidic devices are changing how labs handle embryo selection. These devices manipulate tiny amounts of fluids. They allow scientists to create controlled environments for developing embryos. This leads to better monitoring and selection of viable embryos.
Researchers can now observe cell behavior in real-time. This technology enables them to assess the health and quality of embryos more accurately. Traditional methods often involve guesswork. In contrast, microfluidics provides precise data, helping to choose the best embryos for implantation.
Precision Improvement
Using microfluidic systems enhances precision in IVF procedures significantly. The technology allows for accurate control over the conditions embryos experience. Factors like temperature, pH, and nutrient levels can be finely tuned. This control reduces stress on the embryos during development.
Precision also extends to sperm selection. Microfluidics helps isolate the healthiest sperm cells quickly. It does this by mimicking natural processes that occur in the female reproductive system. This method increases the chances of successful fertilization and embryo development.
Personalized Treatments
Microfluidic technology holds promise for personalized treatment options in IVF. Each patient’s needs are different, and microfluidics can cater to these variations. By analyzing individual cell characteristics, doctors can tailor treatments more effectively.
This personalization can lead to improved patient outcomes. For example, specific protocols can be developed based on a patient’s unique genetic profile. Tailored approaches may enhance success rates and reduce the time spent in treatment.
Future Potential
The future of IVF looks brighter with microfluidic innovations. As research continues, more advanced techniques will emerge. These advancements could lead to higher success rates and healthier pregnancies.
Moreover, integrating artificial intelligence with microfluidics may further enhance embryo selection processes. AI could analyze vast amounts of data quickly, offering insights that human eyes may miss. This combination could revolutionize how fertility specialists approach IVF.
In summary, microfluidic technology transforms the landscape of IVF. It improves embryo selection and culture processes significantly. The benefits of using this technology include enhanced precision in procedures and personalized treatment options that lead to better patient outcomes.
Advances in Fertility Methods
Emerging Techniques
New fertility therapies are emerging alongside traditional IVF methods. These innovations aim to enhance fertility outcomes for couples facing challenges. For instance, preimplantation genetic testing (PGT) allows specialists to screen embryos for genetic disorders before implantation. This approach increases the chances of a successful pregnancy.
Another breakthrough is the use of artificial intelligence in fertility care. AI can analyze data from previous cycles to predict the best times for treatment. This personalized fertility treatment improves success rates and reduces emotional stress for patients.
In Vitro Gametogenesis Impact
In vitro gametogenesis (IVG) is a significant advancement in reproductive technology. IVG allows scientists to create eggs and sperm from stem cells. This method expands reproductive options for those with fertility issues, such as same-sex couples or individuals with medical conditions affecting their gametes.
Research on IVG has gained momentum since its first successful application in 2016. Scientists continue to explore its potential for fertility preservation. By creating gametes from skin cells, IVG offers hope to cancer survivors who may face infertility due to treatments.
Holistic Approaches
Integrating holistic approaches into fertility treatments is essential for improving overall fertility health. Lifestyle modifications play a crucial role in enhancing fertility outcomes. Simple changes like a balanced diet, regular exercise, and stress management can significantly impact reproductive health.
Fertility specialists now recommend these lifestyle adjustments as part of comprehensive fertility care. Studies show that women who maintain a healthy weight and manage stress have higher chances of conception. Combining these holistic strategies with advanced fertility technology creates a more effective treatment plan.
Future Directions
Continued advancements in reproductive technologies promise better solutions for those on their fertility journeys. The focus on personalized fertility treatments aims to address individual needs effectively. As new techniques emerge, the landscape of assisted reproductive technology evolves rapidly.
Innovations such as ovarian tissue freezing provide options for women undergoing medical treatments that may affect their fertility. This technique allows for future use of their own eggs after recovery.
Moreover, ongoing research into gene editing technologies raises ethical questions and possibilities about altering embryos’ genetic makeup. While exciting, these developments require careful consideration and regulation.
Genetic Testing Innovations
Preimplantation Genetic Testing
Recent innovations in preimplantation genetic testing (PGT) have transformed IVF clinics worldwide. PGT allows doctors to analyze embryos for genetic disorders before implantation. This process significantly improves the chances of a successful pregnancy. Clinics now use advanced technologies like next-generation sequencing (NGS). NGS offers precise results and quicker turnaround times.
In 2019, a study showcased how PGT could identify embryos free from common genetic conditions like cystic fibrosis and sickle cell anemia. These advancements help families avoid passing on hereditary diseases. As a result, many couples feel more confident about their choices during IVF.
Ethical Considerations
The rise of genetic testing raises important ethical questions. Some worry about the implications of selecting embryos based on genetic traits. Critics argue it might lead to “designer babies.” They fear this could create social inequality based on genetic selection.
Moreover, there are concerns about privacy and consent. Parents must understand what genetic information means for their future child. Ethical guidelines are essential to navigate these complex issues. Clinics often provide counseling to help parents make informed decisions.
Healthier Pregnancies
Genetic testing can lead to healthier pregnancies. By identifying embryos with potential disorders, parents can choose the healthiest options for implantation. This reduces the risk of complications during pregnancy and childbirth.
Studies show that PGT significantly decreases miscarriage rates linked to chromosomal abnormalities. For instance, research published in 2020 highlighted that women who underwent PGT had a 30% lower chance of miscarriage compared to those who did not.
Parents also report feeling less anxiety when they know their embryos are healthy. They can focus on nurturing their pregnancy without worrying about genetic issues.
Clinical Trials and Future Directions
Clinical trials continue to explore the full potential of genetic testing in IVF. New methods aim to refine embryo selection processes further. Researchers investigate ways to enhance accuracy and reduce costs associated with PGT.
Innovations like artificial intelligence (AI) are being integrated into embryo assessment techniques. AI can analyze vast data sets, improving success rates in selecting viable embryos.
Cryopreservation and Vitrification Techniques
Traditional Cryopreservation
Traditional cryopreservation methods involve slow freezing techniques. This process cools embryos or oocytes gradually. Ice crystals can form during this method. These ice crystals might damage cells and affect survival rates.
Older systems often required the use of cryoprotectants. These substances help prevent ice formation. However, they can also be toxic at high concentrations. As a result, many embryos did not survive after thawing.
Modern Vitrification
Vitrification is a newer technique that uses rapid freezing. This method turns biological materials into a glass-like state without forming ice crystals. The cooling process is much faster than traditional methods.
Vitrification offers several advantages over older methods. First, it significantly increases survival rates after thawing. Studies show that vitrified embryos have higher implantation rates compared to those frozen using traditional techniques.
Second, vitrification allows for better preservation of oocytes. Oocytes are sensitive and can easily be damaged. Vitrification protects them more effectively, making it possible to store them for longer periods.
Impact on IVF Success Rates
Improved cryopreservation methods directly influence IVF success rates. With better preservation techniques, patients have more options. They can choose to freeze their embryos or oocytes without fear of losing quality.
Many clinics now prefer vitrification due to its effectiveness. Patients report higher success rates when using vitrified embryos during IVF cycles. In fact, some studies indicate that pregnancy rates with vitrified embryos can reach up to 70%.
The choice to freeze embryos also empowers patients. It allows them to plan their families according to personal circumstances. For example, women may delay pregnancy for career reasons or health issues.
Patient Choices
Patients now have more choices in their fertility journeys thanks to advancements in cryopreservation technology. They can opt for embryo freezing after successful fertilization or choose to preserve their eggs for future use.
This flexibility is crucial as it aligns with modern lifestyle choices. Many individuals prioritize education and careers before starting families. Improved cryopreservation methods support these decisions by providing safe storage options.
Patients can explore genetic testing innovations alongside these technologies. Combining these approaches enhances the likelihood of successful pregnancies while reducing the risk of genetic disorders.
Role of Deep Learning in IVF
Embryo Viability
Deep learning algorithms play a significant role in analyzing embryo viability. These algorithms process images of embryos to assess their quality. They evaluate factors like shape, size, and development stage. This analysis helps identify which embryos are most likely to result in successful pregnancies.
Clinics now use these advanced technologies to enhance selection processes. The traditional methods relied on human observation, which could be subjective. With deep learning, the evaluation becomes more accurate and consistent. Studies show that AI can improve embryo selection rates by up to 20%. This means a higher chance of successful IVF treatments.
Clinical Decision-Making
AI-driven insights also enhance clinical decision-making in IVF treatments. Medical professionals can access vast amounts of data quickly. They analyze past treatment outcomes and patient histories efficiently. This data helps doctors make informed decisions tailored to individual patients.
For instance, AI can suggest the best protocols for hormone stimulation based on a patient’s unique profile. It can predict how well a patient might respond to treatment. By using these insights, clinics can increase the chances of success while reducing costs.
Ethical Implications
The rise of AI in reproductive medicine raises ethical concerns. Reliance on technology can lead to questions about decision-making authority. Who makes the final call: the doctor or the algorithm? There’s also a risk of over-reliance on technology, which may overlook human intuition.
Privacy is another concern. Collecting and analyzing patient data requires strict security measures. Patients must trust that their information remains confidential. Potential biases in AI algorithms could affect outcomes. If the training data lacks diversity, certain groups may not receive optimal care.
Future Directions
Future advancements in deep learning could further transform IVF practices. Researchers are exploring ways to integrate genetic information into embryo assessment. Combining genetic data with imaging could provide even deeper insights into embryo viability.
Moreover, ongoing studies aim to refine AI algorithms for better accuracy. As technology evolves, so will its applications in reproductive health. Continuous monitoring and adjustment of these systems will be crucial for maintaining ethical standards.
Future Directions and Emerging Trends
Upcoming Innovations
Researchers predict that new technology will transform IVF treatments. Innovations like artificial intelligence and machine learning could enhance embryo selection. These tools may improve success rates by analyzing large data sets of embryo characteristics.
Gene editing is another promising area. Techniques such as CRISPR can potentially eliminate genetic disorders before implantation. This could lead to healthier pregnancies and reduce the risk of inherited diseases.
Moreover, 3D printing is emerging in IVF labs. It allows for the creation of custom-designed culture dishes. These dishes can optimize conditions for embryo development, leading to better outcomes.
Interdisciplinary Collaboration
The advancement of IVF technology relies on collaboration across various fields. Scientists, clinicians, and engineers must work together. Their combined expertise can address complex challenges in reproductive health.
For instance, combining insights from genetics and bioengineering can lead to better understanding of embryo development. This interdisciplinary approach can identify factors that influence success rates in IVF.
Furthermore, partnerships with tech companies can drive innovation. Access to advanced algorithms and data analytics can improve embryo assessment processes. As a result, patients may experience higher success rates with fewer cycles.
Regulatory Adaptation
Regulations must evolve alongside rapid technological advancements in IVF. Legislation often lags behind innovations, creating gaps in patient protection. Continuous adaptation is necessary to ensure safety and ethical standards are met.
New technologies raise questions about consent and privacy. Patients need clear information about how their data will be used. Regulations should address these issues to build trust between patients and providers.
Legislation needs to consider the implications of gene editing. Ethical concerns arise when altering embryos at the genetic level. Lawmakers must balance innovation with the potential risks involved.
States vary widely in their regulations surrounding IVF practices. Some areas have strict laws while others are more lenient. This inconsistency can create confusion for patients seeking treatment options.
Final Remarks
The latest innovations in IVF technology are game-changers. They enhance your chances of conception and improve overall success rates. From microfluidic advancements to deep learning applications, these breakthroughs pave the way for a brighter future in reproductive health. Genetic testing and improved cryopreservation techniques ensure that you have the best options available.
Stay informed about these exciting developments. Your journey through IVF can be more effective and fulfilling with the right knowledge. Explore these advancements further, consult experts, and consider how they can impact your fertility journey. Embrace the possibilities that modern technology offers and take charge of your reproductive health today.
Frequently Asked Questions
What is IVF and why is it important?
IVF, or In Vitro Fertilization, is a fertility treatment that helps couples conceive. It allows for controlled fertilization outside the body, increasing chances of pregnancy, especially for those facing infertility challenges.
What are the latest developments in IVF technology?
Recent advancements include microfluidic technology, improved genetic testing methods, and enhanced cryopreservation techniques. These innovations aim to increase success rates and provide more personalized treatment options for patients.
How does microfluidic technology improve IVF?
Microfluidic technology allows precise manipulation of small fluid volumes. This enhances sperm selection and embryo culture conditions, leading to better fertilization rates and healthier embryos.
What role does genetic testing play in IVF?
Genetic testing identifies chromosomal abnormalities in embryos before implantation. This reduces the risk of genetic disorders and increases the likelihood of successful pregnancies.
What are cryopreservation and vitrification techniques?
Cryopreservation preserves embryos for future use, while vitrification is a rapid freezing method that prevents ice crystal formation. Both techniques enhance storage longevity and maintain embryo viability.
How is deep learning utilized in IVF?
Deep learning algorithms analyze large datasets to predict embryo success rates. This technology improves decision-making in embryo selection, ultimately increasing the chances of successful pregnancies.
What are the future trends in IVF technology?
Emerging trends include personalized medicine approaches, artificial intelligence integration, and advancements in non-invasive testing methods. These innovations aim to optimize IVF outcomes and cater to individual patient needs.
