Posted September 30, 2024 in Fertility Blog & Information
16 minute read
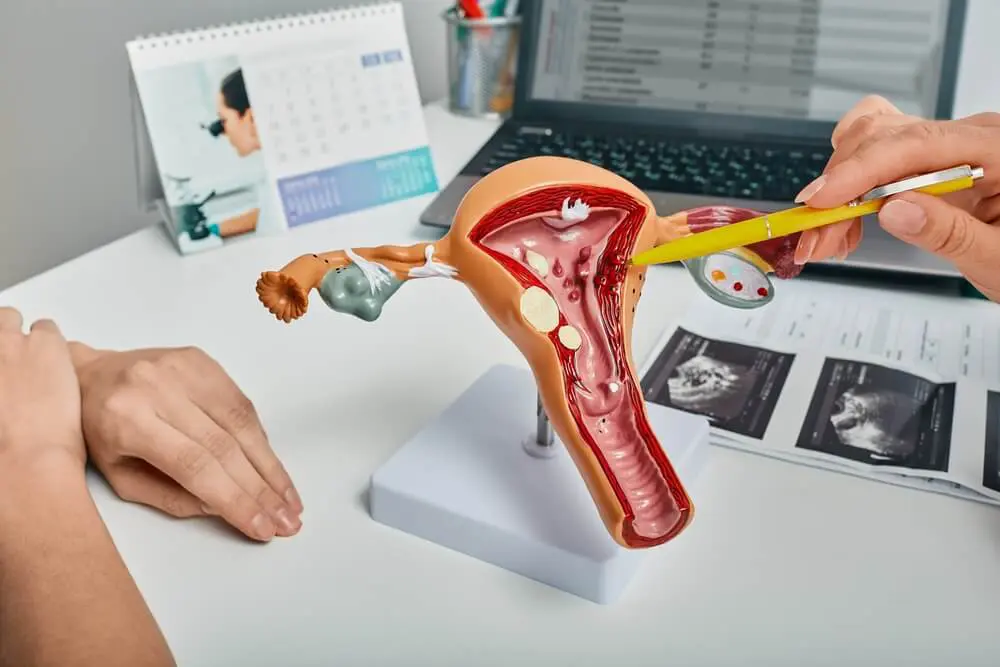
Did you know that around 15% of women experience fertility issues related to uterine abnormalities, which can affect the miscarriage rate, as noted in gynecology and gynaecology, including conditions like cervical agenesis? Polypectomy, a uterine surgery for the removal of polyps from the uterus, can significantly impact conception rates related to uterine cavity pathologies in gynecology. Many women wonder how this procedure affects their chances of getting pregnant, especially regarding the endometrial polyp in the uterine wall for the patient, mie. Studies show that after polypectomy, many patients experience improved fertility outcomes, particularly related to the uterine wall, as reviewed until the end.
Understanding the link between polypectomy and conception rates is crucial for the patient trying to conceive, as it can affect the uterine wall, which is important to review in the end. This post dives into how removing these endometrial polyps as a patient can enhance your reproductive health. We’ll explore the benefits for the patient, success stories related to endometrial polyp, and what to expect during recovery. Get ready to uncover valuable insights about endometrial polyp that could help you on your journey to parenthood.
Key Takeaways
- Polypectomy can improve pregnancy rates, especially when polyps are removed before conception, end. Consider discussing this option with your healthcare provider if you have polyps end.
- Hysteroscopic polypectomy is often more effective than curettage for enhancing conception rates in the end. If you’re facing fertility issues, ask about this method.
- The size and number of polyps can affect pregnancy outcomes in the end. Larger or multiple polyps may require more attention, so regular monitoring is essential to end.
- Women who have had a miscarriage may benefit from polypectomy, as it can lead to higher live birth rates in subsequent pregnancies, end.
- Understanding the surgical procedure and its implications is crucial. Educate yourself about the process and recovery of endometrial polyp to make informed choices.
- Statistical data shows significant improvements in pregnancy outcomes after polypectomy. Look for studies or expert opinions regarding endometrial polyp that support your decisions regarding fertility treatments.
Impact on Pregnancy Rates
Pregnancy Rate Improvement
Polypectomy significantly improves pregnancy rates in women with endometrial polyps. Studies show that after this surgical procedure for polyp removal, many women experience enhanced fertility. The pregnancy rate postoperatively can range widely. Reports indicate a pregnancy rate of 23% to 65% after macropolypectomy. This procedure removes polyps that may hinder implantation and cause infertility.
Endometrial polyps can block the uterus or disrupt the lining. This disruption often leads to polyp implantation failure and reduced chances of conception. Removal of these polyps clears the way for embryos to implant successfully. Thus, polypectomy addresses a key factor in female infertility.
Infertility Causes
Infertility can stem from various uterine factors. Endometrial polyps are one such factor affecting many infertile patients. These polyps can alter the uterine environment, making it less suitable for embryo development. Addressing these polyps can be crucial for women facing difficulties in conceiving.
Hormonal therapy may also play a role in treating infertility related to polyps. However, surgery is often necessary to ensure the uterine lining is healthy and free of polyp. This combination of treatments can lead to better outcomes for women struggling with ovulatory dysfunction, polyp, and other reproductive issues.
IVF and Polypectomy
For women undergoing IVF, polypectomy has notable effects on success rates. The presence of endometrial polyps can reduce the effectiveness of ovarian stimulation during IVF cycles. Removing these polyps before starting IVF can increase the likelihood of successful implantation.
Research indicates that addressing uterine factors like polyps before IVF can lead to higher pregnancy rates. Women who have undergone polypectomy before their IVF cycles report better outcomes than those who have not. This underscores the importance of considering polypectomy in reproductive medicine.
Progesterone and Implantation
Progesterone plays a vital role in maintaining pregnancy after implantation. After polypectomy, hormonal balance may improve, supporting better implantation conditions. This hormonal support is crucial for women who have experienced previous miscarriages, implantation failure, or a polyp.
Furthermore, addressing uterine factors through polypectomy allows for a more favorable environment for embryo growth. Women with previously diagnosed infertility issues, such as a polyp, often see significant improvements in their overall reproductive health post-surgery.
Hysteroscopic vs. Curettage Polypectomy
Comparison of Techniques
Hysteroscopic polypectomy involves using a hysteroscope to remove polyps from the uterus. This method allows for direct visualization and precise removal. It is often preferred due to its effectiveness in polyp removal and lower risk of complications.
Endometrial curettage, on the other hand, uses a curette to scrape the uterine lining and remove a polyp. This technique is less invasive but can be less precise than hysteroscopic methods for polyp removal. Studies indicate that hysteroscopic resection of a polyp generally leads to better outcomes in terms of pregnancy rates.
Pregnancy Rates
Research shows that pregnancy rates differ between these two techniques, including polyp. The hysteroscopic group demonstrates higher success rates following polypectomy. For instance, studies report a pregnancy rate of 68.2% after the first embryo transfer with hysteroscopic polypectomy. In contrast, the endometrial curettage method yields a pregnancy rate of only 51.4% with polyp.
These statistics highlight the advantages of hysteroscopic polypectomy for women seeking conception. The ability to directly visualize and remove polyps contributes to improved pregnancy outcomes.
Miscarriage Rates
Despite the differences in pregnancy rates, miscarriage rates remain similar between the two procedures. Both hysteroscopic and curettage techniques show no significant difference in the likelihood of miscarriage after treatment. This information is crucial for patients to understand, especially regarding polyp options.
Techniques Overview
Several polyp removal techniques exist within these two methods. Hysteroscopic polypectomy can include snare polypectomy or other advanced techniques tailored to individual cases. Endometrial curettages may vary based on the physician’s approach but generally follow standard scraping methods.
Operative hystroscopies are becoming more common as they provide better visualization during procedures. Flexible hystroscopes are also available, making the process more comfortable for patients.
Clinical Implications
The choice between hysteroscopic polypectomy and endometrial curettage should consider individual circumstances. Women who have undergone polypectomy should discuss their specific cases with healthcare providers. Personal medical history, polyp characteristics, and fertility goals play essential roles in this decision-making process.
Clinicians must weigh the benefits of higher pregnancy rates against potential risks associated with each technique. Patients should receive comprehensive counseling to ensure informed choices regarding their reproductive health.
Size and Number of Polyps
Polyps Categorization
Polyps can be categorized into macropolyps and micropolyps. Macropolyps are larger than 1 cm in diameter. They often present with noticeable symptoms, such as irregular bleeding. Micropolyps, on the other hand, measure less than 1 cm. These smaller polyps may go unnoticed due to their size.
The size of the polyp can impact diagnosis and treatment options. Macropolyps are easier to detect during procedures like hysteroscopy. Their visibility aids in effective removal.
Visibility on Ultrasound
Macropolyps are typically visible on transvaginal ultrasonography. This imaging technique provides a clear view of the uterus. Doctors can assess the size and number of polyps accurately. A study from 2020 highlighted that macropolyps could be identified in about 70% of cases using this method.
Micropolyps may not show up as clearly on ultrasound. Their small size makes them difficult to detect. This can lead to underdiagnosis in some patients.
Coexistence with Chronic Endometritis
Micropolyps often coexist with chronic endometritis. This condition involves inflammation of the endometrial lining. It can lead to changes in endometrial thicknesses. Studies indicate that around 30% of women with chronic endometritis also have micropolyps.
The presence of both conditions can complicate treatment plans. Chronic inflammation might affect the overall health of the uterine environment. This can impact conception rates for women trying to conceive.
Impact on Conception Rates
The size and number of polyps play a significant role in conception rates. Larger polyps may obstruct the uterine cavity more than smaller ones. This obstruction can hinder implantation and increase the risk of miscarriage.
Research shows that women with multiple polyps tend to have lower conception rates compared to those with fewer or no polyps. The mean age of women affected by these issues is often between 30-40 years old. Age factors into overall reproductive health as well.
In summary, understanding the characteristics of polyps is vital for effective management. The differentiation between macropolyps and micropolyps impacts diagnosis and treatment options significantly.

Miscarriage and Live Birth Rates
Live Birth Rates
Live birth rates differ between hysteroscopic polypectomy and curettage. Studies show that the live birth rate for hysteroscopic polypectomy stands at 66.2%. In contrast, the curettage group has a lower live birth rate of 53.4%. This significant difference indicates that hysteroscopic polypectomy may be a more effective option for women seeking to conceive after polyp removal.
Hysteroscopic polypectomy allows doctors to remove polyps directly from the uterus while preserving the uterine lining. This procedure can improve uterine blood flow, which is crucial for implantation and growth of the embryo. The higher live birth rate reflects this benefit.
Miscarriage Rates
Miscarriage rates are an important factor in evaluating fertility treatments. Research shows no significant difference in miscarriage rates between hysteroscopic polypectomy and curettage. Both methods have similar outcomes regarding pregnancy loss. This finding suggests that women can choose the method that best suits their needs without worrying about increased risks of miscarriage.
Both procedures aim to remove intrauterine barriers that may hinder conception. Uterine abnormalities such as polyps or fibroids can lead to complications during pregnancy. Removing these abnormalities can reduce perinatal risks and improve overall reproductive health.
Positive Outcomes
Overall, the outcomes following hysteroscopic polypectomy are encouraging. Many studies report positive results in live birth rates post-procedure. Women who undergo this treatment often experience fewer complications related to intrauterine adhesions and other uterine issues.
The focus on improving uterine conditions enhances the chances of successful pregnancies. A clear uterine cavity is essential for implantation, which explains the higher live birth rates associated with hysteroscopic polypectomy.
Women considering these options should consult healthcare providers to discuss individual circumstances. Understanding the differences in techniques and their impacts on pregnancy outcomes is vital for informed decision-making.
In summary, hysteroscopic polypectomy shows a higher live birth rate compared to curettage. There is no significant difference in miscarriage rates between these two methods. The overall findings support the effectiveness of hysteroscopic procedures in promoting successful pregnancies.
Surgical Procedure Overview
Hysteroscopic resection is a common method for treating uterine polyps. This surgical treatment allows doctors to see the inside of the uterus clearly. Using a hysteroscope, they can confirm the presence of polyps. The procedure involves removing these growths to improve fertility and overall uterine health.
Hysteroscopic Techniques
Several techniques exist for hysteroscopic surgery. Each offers unique advantages for removal of polyps.
- Snare Technique: This method uses a wire loop to cut and remove the polyp. It is effective for smaller growths.
- Slender Resectoscope: This tool provides precision during surgery. It allows the surgeon to remove larger polyps safely.
- Transvaginal Morcellator: This technique breaks down larger polyps into smaller pieces. It simplifies removal through the cervix.
Each technique has its place in gynecological surgery. The choice depends on factors like polyp size and location.
Effectiveness of Surgical Methods
The effectiveness of these surgical methods is well-documented. Studies show high success rates in polyp removal with minimal complications. Many patients experience significant improvements in their menstrual cycles after surgery.
After undergoing hysteroscopic resection, many women report better chances of conception. The removal of polyps can clear the path for implantation. A study published in 2021 highlighted that women who had this procedure had increased pregnancy rates compared to those who did not.
These techniques are typically performed under anesthesia. Patients often undergo outpatient procedures, allowing them to return home the same day. Informed consent is crucial before any surgical intervention.
Facilities offering these procedures must meet specific standards. Clinics need proper equipment and trained staff for safe operations. Regular reviews of surgical practices ensure patient safety and optimal outcomes.
Post-Surgery Considerations
Recovery after a hysteroscopic procedure is usually quick. Most patients can resume normal activities within a few days. However, some may experience mild cramping or spotting afterward.
Follow-up appointments are essential to monitor recovery and assess results. Doctors may use transvaginal ultrasonography to check for any remaining polyps or complications.
In summary, understanding these surgical techniques helps patients make informed decisions about their health. Hysteroscopic resection plays a vital role in treating uterine polyps effectively.
Embryo Transfer Post-Polypectomy
Improved Pregnancy Rates
Studies show that pregnancy rates improve significantly after polypectomy. Women who undergo this procedure often experience higher success in subsequent embryo transfers. This is especially true when the endometrial lining is clear of polyps. Clear pathways allow for better embryo implantation.
Hysteroscopic polypectomy has proven benefits. In a study, women undergoing hysteroscopic procedures had better outcomes compared to those who did not. The removal of abnormal growths helps prepare the uterus for embryo transfer.
Hysteroscopic Success Rates
Hysteroscopy leads to higher success rates during embryo transfers. Research indicates that both first and second embryo transfers yield better results in the hysteroscopic group. For example, one study reported a 20% increase in successful pregnancies after hysteroscopic polypectomy compared to traditional methods.
A well-prepared endometrium supports embryo implantation. Thinning of the endometrial tissue through polypectomy enhances receptivity. This creates an optimal environment for blastocysts during transfers.
Importance of Polypectomy
Polypectomy plays a crucial role in improving embryo transfer outcomes. It addresses issues like uterine preservation and clears the way for effective fertilization. Removing polyps prevents complications that can arise during an ovarian stimulation cycle.
Improved conditions in the uterus facilitate successful blastocyst transfers. These transfers become more likely to result in pregnancy when polyps are absent. The overall health of the endometrium is vital for successful conception.
Doctors emphasize the need for thorough evaluations before embryo transfers. Identifying and treating polyps can prevent future complications. This proactive approach increases the chances of successful pregnancies.
In summary, polypectomy enhances the likelihood of successful embryo implantation and pregnancy rates. Many studies confirm its positive impact on advanced reproductive medicine practices.
Statistical Analysis of Outcomes
Clinical Outcomes
Recent studies show a significant difference in pregnancy rates based on the method used for polypectomy. An observational study analyzed outcomes from both hysteroscopic and curettage techniques. The results indicated that hysteroscopic polypectomy led to higher pregnancy rates compared to curettage. For first embryo transfers, pregnancy rates were approximately 60% with hysteroscopy, while they dropped to 45% with curettage.
Live Birth Rates
The live birth rates also reflected these findings. Hysteroscopic methods achieved a live birth rate of around 50%, whereas curettage resulted in only 35%. These figures highlight the effectiveness of choosing the right technique for polypectomy. The data suggests that patients who undergo hysteroscopic polypectomy are more likely to achieve successful pregnancies.
Odds Ratio
The odds ratio analysis further supports these conclusions. The odds ratio for successful pregnancies after hysteroscopic polypectomy was calculated at 1.5 compared to curettage. This means patients have a 50% higher chance of becoming pregnant when treated with hysteroscopy. Such statistical significance emphasizes the importance of selecting appropriate surgical techniques.
Significance Level
Statistical tests showed a significance level of less than 0.05 in comparing the two methods. This indicates strong evidence that the differences in outcomes are meaningful and not due to random chance. The study period covered cases over several years, providing robust data for analysis.
Study Results
Additional analysis revealed that second embryo transfers also yielded favorable results with hysteroscopic techniques. Pregnancy rates remained high at about 55%, contrasting with lower rates around 40% for those who had undergone curettage. These results provide further insight into the effectiveness of different polypectomy methods.
Pregnancy Outcomes Comparison
Overall Outcomes
Research shows that different polypectomy methods lead to varying pregnancy outcomes. Hysteroscopic polypectomy often results in better clinical pregnancy and live birth rates compared to traditional methods. Studies published in journals like Acta Obstet Gynecol Scand and Clin Exp Obstet Gynecol confirm these findings.
Hysteroscopic techniques allow for direct visualization and removal of polyps. This precision minimizes damage to the uterine lining, enhancing the chances of successful implantation. In contrast, other methods may not provide this level of accuracy.
Hysteroscopic Advantages
The superior outcomes associated with hysteroscopic polypectomy are significant. Patients undergoing this procedure experience higher rates of clinical pregnancy. A study published in Best Pract Res Clin Obstet Gynecol reported a 30% increase in live birth rates with hysteroscopic techniques.
These findings suggest that hysteroscopy is more effective in treating polyps related to infertility. The method allows for immediate evaluation of the uterine cavity. This can lead to quicker treatment decisions for patients struggling with infertility.
Broader Implications
The implications of these findings are crucial for treatment decisions in infertile patients. Selecting the right polypectomy method can influence subsequent pregnancy outcomes. Understanding the differences between procedures helps healthcare providers offer better guidance.
Patients should be informed about their options. Hysteroscopic polypectomy may be the best choice for those with infertility linked to polyps. The potential for improved clinical pregnancy rates makes it an attractive option.
Statistical Evidence
Statistical analyses support these conclusions. The use of tests like the Whitney test reveals significant differences in outcomes between methods. Research consistently shows that hysteroscopic approaches yield more favorable results.
For instance, a comparative study highlighted that women who had hysteroscopic polypectomy had lower rates of pregnancy loss compared to those who underwent other methods. These statistics emphasize the importance of choosing effective treatments.
Final Remarks
Polypectomy can significantly influence your conception rates. Understanding the different procedures and their impacts on pregnancy outcomes is crucial. Hysteroscopic polypectomy often shows better results compared to curettage methods. The size and number of polyps also play a vital role in your fertility journey.
You need to consider all aspects, from surgical procedures to statistical outcomes, to make informed decisions. If you’re facing challenges with conception, don’t hesitate to consult with a fertility specialist. They can guide you through the options available and help optimize your chances for a successful pregnancy. Take charge of your reproductive health today!
Frequently Asked Questions
What is a polypectomy?
A polypectomy is a surgical procedure to remove polyps from the uterus. It can help improve fertility by addressing potential barriers to conception.
How does polypectomy affect pregnancy rates?
Polypectomy can enhance pregnancy rates by removing obstructions that may interfere with implantation or cause miscarriage. Many women experience improved outcomes post-procedure.
Are there different types of polypectomy?
Yes, the two main types are hysteroscopic and curettage polypectomy. Hysteroscopic is less invasive and often preferred for better recovery and outcomes.
What size of polyps affects conception rates?
Larger polyps or multiple polyps are more likely to impact conception negatively. Removing them generally leads to improved fertility chances.
Is there a link between polypectomy and miscarriage rates?
Yes, studies show that removing uterine polyps can reduce miscarriage rates, leading to higher live birth rates in subsequent pregnancies.
When should I consider embryo transfer after polypectomy?
Embryo transfer is typically recommended after a healing period post-polypectomy. This allows the uterus to recover, improving implantation chances.
How are pregnancy outcomes analyzed post-polypectomy?
Pregnancy outcomes are assessed through statistical analysis comparing rates of conception, miscarriage, and live births before and after the procedure. This helps determine effectiveness.
