Posted December 16, 2024 in Fertility Blog & Information
17 minute read

Did you know that about 1 in 6 men who have had a vasectomy later seek fertility treatment options, including testicular sperm aspiration and complicated vasoepididymostomy, to address issues with sperm parts and testicular vessels? This surprising statistic highlights the reality for many couples wanting to expand their families. Fortunately, there are effective solutions available.
From vasectomy reversal to sperm retrieval techniques, various fertility treatment options, part of the ductus arteries muscle, can help restore your chances of conceiving. Each method has its pros and cons, making it essential to understand what works best for your unique situation. With the right information and guidance, you can navigate this journey with confidence. Explore these options and take the first step toward growing your family today.
Key Takeaways
- If you’re considering fertility options after a vasectomy, start by understanding the implications of the procedure on your fertility and the available treatments.
- Explore vasectomy reversal as a potential option; it may restore natural fertility for some men, but results can vary.
- Look into sperm retrieval techniques if reversal is not suitable; methods like TESA or PESA can help collect sperm directly from the testicles.
- In vitro fertilization (IVF) can be an effective method for achieving pregnancy after a vasectomy, especially when combined with sperm retrieval.
- Don’t overlook the emotional aspects of this journey; seeking support from professionals or support groups can be beneficial.
- Always consult a fertility specialist to discuss your specific situation and tailor a treatment plan that suits your needs.
Understanding Vasectomy and Fertility
Definition of Vasectomy
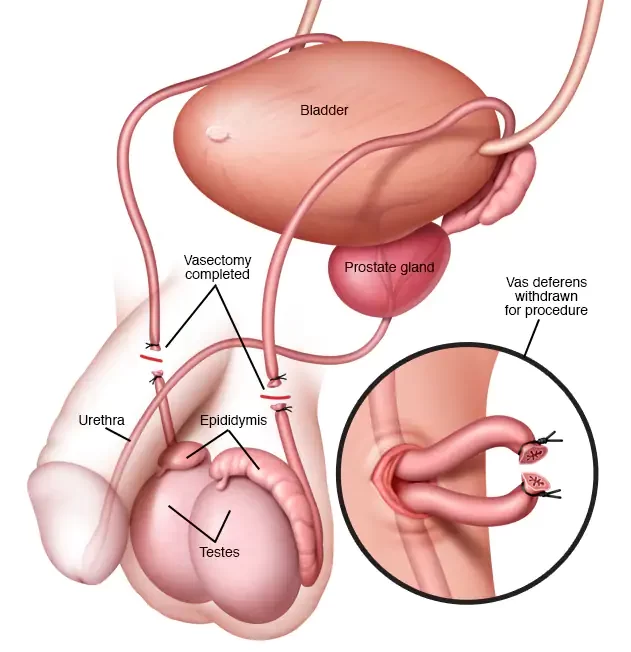
Vasectomy is a surgical procedure. It serves as a permanent method of contraception for men. During the procedure, doctors cut and seal the vas deferens. This is the tube that carries sperm from the testicles to the urethra. Once this tube, the vas, is blocked, sperm cannot mix with semen during ejaculation.
The primary purpose of a vasectomy is to prevent pregnancy. Many men choose this option when they feel complete with their families, vas. It’s important to note that vasectomy does not affect sexual function or testosterone levels.
Impact on Sperm Transport
After a vasectomy, sperm cannot travel through the vessels. The sealed vas deferens stops sperm from reaching the semen. Instead, sperm continues to be produced in the testicles but has no way to exit the body through the vas.
This leads to a buildup of sperm in the vas testicles. The body eventually absorbs this excess sperm over time. Male infertility results from this blockage. Men who undergo this procedure will not father children naturally unless further steps are taken.
Fertility Restoration Options
Fertility restoration after a vasectomy is possible through various methods. One common approach is a vasectomy reversal. This surgery reconnects the severed ends of the vas deferens. Success rates vary based on how long it has been since the original vas procedure.
Another option is sperm retrieval techniques. These methods include percutaneous epididymal sperm aspiration (PESA) and testicular sperm extraction (TESE). These techniques allow doctors to collect sperm directly from the testicles, vas, or epididymis.
Men considering these options should consult with a specialist. A healthcare provider can assess individual cases and recommend suitable treatments, vas.
Studies show that about 50% of men who have a vas reversal surgery achieve pregnancy within three years. However, factors like age and time since vasectomy play significant roles in success rates.
Initial Steps for Fertility Consideration
Evaluate Readiness
Personal readiness is crucial after a vasectomy. Many men reflect on their desires for children. Some may change their minds about fatherhood later in life, vas. It’s important to assess emotional and financial readiness. Consider the impact of having children on your current lifestyle. Discuss these feelings with a partner or trusted friend.
The desire for children can be strong, even after a vasectomy. Understanding this desire helps in making informed decisions about fertility options, vas. Write down thoughts and feelings regarding parenthood. This exercise can clarify your intentions.
Research Options
Gathering information on fertility treatment options is essential. Various methods are available to restore fertility after a vasectomy. Common procedures include vasectomy reversal and sperm retrieval techniques.
Vasectomy reversal involves reconnecting the reproductive organs. This vas surgery aims to restore the flow of sperm through the reproductive system. Success rates vary based on factors like time since the vasectomy and age.
Sperm retrieval techniques involve collecting sperm directly from the testicles, vas, or epididymis. Methods such as Testicular Sperm Extraction (TESE) and Percutaneous Epididymal Sperm Aspiration (PESA) are common. These options can help if a reversal is not possible or desired.
Research also includes understanding costs, recovery times, and potential risks associated with each vas procedure. Online resources and medical literature provide valuable insights into these treatments.
Consult Healthcare Provider
Consulting with a healthcare provider is a vital step in this process. A doctor can evaluate individual circumstances and health conditions. They will discuss the best options based on personal medical history.
During consultations, ask questions about the procedures you are considering. Discuss potential outcomes and any concerns you may have about the reproductive organs involved in these treatments.
Understanding how these procedures work helps set realistic expectations. A healthcare provider can also refer you to specialists if needed.
It’s essential to consider lifestyle factors that might affect fertility treatment success. Factors like smoking, alcohol consumption, and overall health play significant roles in reproductive health.
Healthcare providers often recommend tests before proceeding with any treatment. Tests may include hormone levels, semen analysis, or imaging studies to assess the arteries supplying blood to the reproductive organs.
Exploring Vasectomy Reversal
Procedure Overview
Vasectomy reversal involves surgical procedures to reconnect the vas deferens. Two main techniques are used: vasovasostomy and vasoepididymostomy.
In a vasovasostomy, the surgeon reconnects the two ends of the vas deferens. This is often performed when the obstruction is close to where the original vasectomy occurred. The procedure typically takes about two to four hours.
If there is blockage at the epididymis, a vasoepididymostomy may be necessary. This connects the vas deferens directly to the epididymis. Surgeons may also perform an intussuscepted vasoepididymostomy for more complicated cases.
Surgeons use microsurgical techniques to enhance precision. They employ magnification tools to ensure accuracy. This helps reduce complications and improve recovery.
Success Rates
Several factors influence the success rates of vasectomy reversals. Time since the original procedure plays a significant role. Generally, success rates decrease as more years pass after the vasectomy.
Age also impacts outcomes. Younger men tend to have higher success rates than older men. The quality of sperm production can decline with age.
The surgeon’s experience matters too. Skilled surgeons achieve better results than those with less experience.
Other factors include the health of the vas deferens mucosa and the condition of surrounding structures like seminal vesicles and ejaculatory ducts. If these areas are healthy, chances improve significantly.
Benefits vs Limitations
Reversal offers specific benefits compared to other fertility options. One major advantage is restoring natural fertility without invasive procedures like IVF. Couples can conceive naturally, which many find appealing.
However, there are limitations to consider. Reversal surgery does not guarantee pregnancy. Success rates vary widely based on multiple factors mentioned earlier.
Costs can be high for reversal surgery, and insurance may not cover it. Alternative options like sperm retrieval or IVF exist but come with their own set of challenges and expenses.
Sperm retrieval methods, such as TESE (testicular sperm extraction), can provide sperm directly from the testicles if reversal fails. IVF can then be used for fertilization, but it requires additional steps and costs.
Couples must weigh these factors carefully before deciding on a path forward.
Sperm Retrieval Techniques
Surgical Methods
Surgical sperm retrievals are essential when a vasectomy prevents natural ejaculation. Two common techniques are Testicular Sperm Extraction (TESE) and Microdissection Epididymal Sperm Aspiration (MESA).
TESE involves removing tissue from the testicles. Doctors then extract sperm from this tissue. This method is useful when sperm production is normal, but the sperm duct is blocked.
MESA targets the epididymis, the tube where sperm matures. Surgeons use a fine needle to aspirate fluid that contains sperm. MESA is effective for men with obstructed sperm ducts. Both methods can yield viable sperm for further procedures.
Obstruction Scenarios
Certain situations require sperm retrieval due to obstruction in the reproductive tract. A common cause is a previous vasectomy. Other causes include congenital absence of the vas deferens or infections that affect the spermatic cord.
In these cases, retrieving sperm becomes crucial for fatherhood. Without these methods, men may not have any viable sperm for assisted reproduction. Understanding the underlying issues helps doctors decide on the best approach.
Assisted Reproductive Technologies
Retrieved sperm can be utilized in various assisted reproductive technologies (ART). One popular method is Intracytoplasmic Sperm Injection (ICSI). This technique involves injecting a single sperm directly into an egg.
ICSI enhances fertilization chances, especially when sperm motility is low. It allows couples to achieve pregnancy even with limited or damaged sperm. Other methods include In Vitro Fertilization (IVF), where eggs and sperm combine outside the body.
Using ART opens doors for many families facing fertility challenges after a vasectomy. The success rates vary based on individual circumstances and health factors.
In Vitro Fertilization Overview
IVF Concept
In vitro fertilization (IVF) is a widely recognized fertility treatment. It allows couples to conceive when other methods fail. This process involves collecting eggs from the woman and sperm from the man. The eggs and sperm are combined in a laboratory setting to create embryos.
IVF provides an option for men who have undergone a vasectomy. Sperm retrieval techniques can be used to obtain sperm directly from the epididymis or testicles. This method ensures that viable sperm are available for fertilization.
IVF Process
The IVF process begins with ovarian stimulation. A doctor prescribes hormones to encourage the ovaries to produce multiple eggs. Once the eggs mature, they are retrieved through a minor surgical procedure.
The next step is fertilization. The retrieved eggs are placed in a dish with sperm. Fertilization usually occurs within hours. After fertilization, embryos develop for several days before being transferred to the woman’s uterus.
Sperm retrieval plays a critical role in this process for post-vasectomy patients. Techniques like percutaneous epididymal sperm aspiration (PESA) or testicular sperm extraction (TESE) may be employed. These methods allow doctors to access sperm even when it is not present in the semen due to the vasectomy.
Success Rates
Success rates for IVF vary based on several factors. Age is a significant factor; younger women typically have higher success rates. According to the Centers for Disease Control and Prevention (CDC), the average live birth rate per IVF cycle is about 30% for women under 35 years old.
For post-vasectomy patients, success rates also depend on sperm quality and retrieval method. If healthy sperm are obtained, chances of successful fertilization increase. However, it’s essential to note that not all embryos will implant successfully after transfer.
Considerations
Several considerations exist for couples considering IVF after a vasectomy. Financial costs can be substantial, as IVF often requires multiple cycles for success. Insurance coverage varies widely, so patients should check their plans.
Emotional stress can also be a factor during this journey. Support from counseling or support groups may help couples cope with the ups and downs of treatment.
Patients should discuss all options with their healthcare provider before proceeding with IVF. Understanding the entire process, including potential risks and benefits, is crucial for informed decisions.
Achieving Pregnancy Post-Vasectomy
Timeline for Treatment
Achieving pregnancy after a vasectomy involves several steps. First, men need to consult with a fertility specialist. This consultation typically happens within a few weeks of deciding to pursue treatment.
The first option is vasectomy reversal, which can take 2-4 hours. This surgery reconnects the vas deferens tubes. Recovery takes about 1-2 weeks. After recovery, doctors usually suggest waiting 3-6 months before testing sperm count.
Another option is sperm retrieval for in vitro fertilization (IVF). This process can be done via testicular sperm extraction (TESE) or percutaneous epididymal sperm aspiration (PESA). Both procedures can occur quickly, often within a few days of the initial consultation.
Importance of Coordination
Timing and coordination with specialists are crucial during this process. Fertility specialists guide couples through each step. They help choose the best option based on individual circumstances.
Regular follow-ups are essential. Specialists monitor hormone levels and sperm quality over time. These check-ups provide valuable insights into the effectiveness of treatments. Couples should communicate openly with their doctors about concerns or changes in health.
Challenges and Solutions
Several challenges may arise during conception after a vasectomy. One common issue is low sperm count post-reversal or retrieval. In such cases, IVF can be an effective solution. This method allows doctors to use retrieved sperm for fertilization.
Emotional stress also plays a role in this journey. Couples may feel anxious or frustrated if conception takes longer than expected. Seeking support from counselors or support groups can help manage these feelings.
Financial concerns may arise as well. Treatments like IVF can be costly and may not always be covered by insurance. Exploring financing options or discussing payment plans with clinics can ease this burden.
Lastly, physical challenges can occur, such as complications from surgery. It’s vital to discuss any risks with the surgeon beforehand. Understanding potential outcomes helps manage expectations.
Coping with Emotional Impact
Emotional Challenges
Fertility issues can create significant emotional stress. Individuals may feel sadness, frustration, or even anger after a vasectomy. These feelings are normal. They often stem from the desire to have children and the unexpected challenges that arise. The journey to parenthood can feel daunting. This is especially true when faced with medical interventions like aspiration or surgical procedures.
Couples might experience tension in their relationship. The pressure of infertility can lead to misunderstandings. Partners may not know how to express their feelings. This silence can deepen emotional wounds. Open communication is vital in these situations. Sharing thoughts and concerns helps build a supportive environment.
Coping Strategies
Several coping strategies can help individuals and couples navigate these emotions. First, seeking professional help is important. A therapist specializing in fertility issues can provide guidance. They can help couples process their feelings and develop coping mechanisms.
Support groups also offer valuable resources. Connecting with others facing similar challenges creates a sense of community. Sharing experiences can lighten the emotional burden. Couples may find comfort in knowing they are not alone.
Practicing self-care is another key strategy. Engaging in activities that promote relaxation can be beneficial. This could include yoga, meditation, or spending time outdoors. Physical activity releases endorphins, which improve mood and reduce stress.
Open Communication
Open communication about feelings is essential for managing the emotional impact of fertility issues. Couples should discuss their hopes and fears regarding treatment options and future family plans. Honest conversations foster understanding and empathy between partners.
Discussing the various fertility treatment options available after a vasectomy is crucial too. Exploring methods like reversal surgery or sperm retrieval can provide clarity on the next steps. Knowing what to expect during these procedures helps ease anxiety.
By addressing emotions openly, couples strengthen their bond. They learn to support each other through this challenging time. Encouragement and understanding become cornerstones of their relationship.
Seeking Support
Finding support from friends and family can also make a difference. Loved ones can provide comfort during difficult moments. They often offer a listening ear or practical help when needed.
Consider joining online forums or local community groups focused on fertility issues. These platforms allow for sharing resources and personal stories. Many people find strength in shared experiences.
Consult a Fertility Specialist
Importance of Consultation
Consulting a fertility specialist is crucial after a vasectomy. These professionals provide personalized advice tailored to individual circumstances. They understand the complexities involved in fertility treatments. A specialist can explain various options available for achieving pregnancy.
A consultation helps clarify what steps to take next. Specialists assess medical history, including any issues with the uterus or prostate. They also evaluate other factors that could affect fertility, such as kidney function and blood health. This thorough evaluation leads to better-informed decisions.
Questions to Ask
During the consultation, it’s important to ask specific questions. Here are some key inquiries:
- What are my treatment options after a vasectomy?
- How do these treatments work?
- What are the success rates for each option?
- Are there any risks involved?
- How long will the treatment process take?
Asking these questions can help you understand your choices clearly. The answers will guide you in making informed decisions about your fertility journey.
Ongoing Follow-Up
Follow-up appointments are essential throughout this process. Regular check-ins with your specialist ensure that everything is on track. These visits provide opportunities to discuss progress and any concerns that may arise.
Support from healthcare providers is vital during this time. Specialists can monitor hormone levels and other factors affecting fertility. They can also offer emotional support, which is important after experiencing the challenges of infertility.
Emotional Support
Fertility treatments can be emotionally taxing. Having an ongoing relationship with a specialist can ease some of this burden. Their expertise provides reassurance during uncertain times.
Consider joining support groups or counseling services as well. Sharing experiences with others who face similar challenges can be beneficial. It creates a sense of community and understanding.
Summary
Consulting a fertility specialist plays a key role in navigating options after a vasectomy. Personalized advice is important for making informed decisions about treatment paths. Asking the right questions during consultations clarifies available options and their implications.
Ongoing follow-up ensures continuous support throughout the journey toward parenthood. Emotional well-being matters just as much as physical health in this process.
Remarks Finales
Navigating fertility treatment options after a vasectomy can feel overwhelming. You’ve got choices like vasectomy reversal, sperm retrieval, and in vitro fertilization. Each path has its pros and cons, but understanding them empowers you to make informed decisions for your family’s future.
Don’t let emotional challenges hold you back. Seek support from specialists who can guide you through this journey. Your dreams of parenthood are within reach. Take that first step today by consulting a fertility expert. Explore your options and reclaim your fertility journey with confidence.
Frequently Asked Questions
What is a vasectomy?
A vasectomy is a surgical procedure that cuts or blocks the vas deferens, preventing sperm from mixing with semen. It’s considered a permanent form of male contraception.
Can I still father children after a vasectomy?
Yes, you can still father children after a vasectomy. Options include vasectomy reversal or assisted reproductive technologies like sperm retrieval and in vitro fertilization.
How long after a vasectomy can I consider fertility treatments?
You can explore fertility treatments immediately after deciding to have children again. However, it’s best to consult a specialist for personalized advice based on your circumstances.
What are the chances of successful vasectomy reversal?
Success rates for vasectomy reversal vary but typically range from 50% to 90%. Factors like time since the procedure and the surgeon’s expertise play crucial roles.
What is sperm retrieval?
Sperm retrieval is a process used to collect sperm directly from the testicles or epididymis. This is often done if a vasectomy reversal isn’t possible or desired.
How does in vitro fertilization work post-vasectomy?
In vitro fertilization (IVF) involves retrieving eggs from a partner, fertilizing them with retrieved sperm, and implanting embryos into the uterus. It bypasses the need for natural sperm transport.
Should I consult a fertility specialist after a vasectomy?
Absolutely. A fertility specialist can provide tailored advice and treatment options based on your health history and family planning goals. They help optimize your chances of conception.
