Posted November 29, 2024 in Fertility Blog & Information
16 minute read

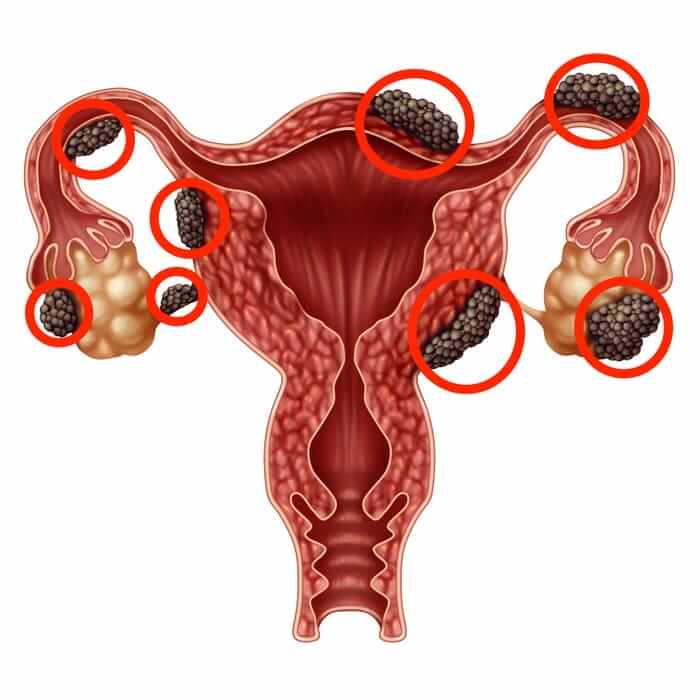
About 1 in 10 women worldwide suffer from endometriosis, a condition that can significantly impact fertility. This often-painful disorder leads to the growth of tissue similar to the lining inside the uterus, causing various complications. Fortunately, innovative treatments are emerging that can help improve fertility for those affected by endometriosis pain, endometriosis tissue, and endometriosis growth.
From hormonal therapies to advanced surgical techniques, options for fertility treatment and managing endometriosis pain are becoming more effective and personalized, targeting endometriosis tissue. These treatments aim to reduce symptoms and enhance reproductive potential. Understanding these advancements is crucial for anyone navigating the challenges of endometriosis. With the right approach, hope for improved fertility is on the horizon.
Key Takeaways
- Understanding endometriosis is crucial for improving fertility; recognizing symptoms can lead to earlier diagnosis and treatment options.
- Surgical treatments can significantly enhance fertility by removing endometrial tissue, so consider discussing this option with your healthcare provider.
- Medical approaches, including hormone therapy, can help manage symptoms and improve chances of conception; explore these options with a specialist.
- For those in early stages, Clomiphene IUI is a recommended method that can effectively stimulate ovulation and increase pregnancy rates.
- Advanced stages may require more complex interventions, such as In-Vitro Fertilization (IVF), which has proven successful for many women facing infertility due to endometriosis.
- Don’t overlook supportive treatments like nutrition and stress management; they play a vital role in overall reproductive health and can complement medical interventions.
Understanding Endometriosis and Fertility
Definition and Prevalence
Endometriosis affects about 10% of women during their reproductive years. This condition occurs when tissue similar to the lining inside the uterus grows outside it. Women can experience various symptoms, including severe endometriosis pain, heavy periods, and fatigue. The exact cause remains unclear, but genetics and hormonal factors may play a role.
Impact on Fertility
Women with endometriosis often face fertility challenges. The endometriosis experience infertility is common among those diagnosed with this condition. Anatomical changes caused by endometriosis can block fallopian tubes or distort pelvic anatomy. Deep endometriosis may affect nearby organs such as the ovaries or bladder. Bowel endometriosis can also lead to complications that impact fertility.
Research shows that the endometriosis fertility index (EFI) helps assess a woman’s chances of conception. This tool evaluates various factors like age, duration of infertility, and previous pregnancies. A lower EFI indicates a higher risk of infertility.
Importance of Early Diagnosis
Early diagnosis plays a crucial role in managing fertility issues related to endometriosis. Many women suffer for years before receiving a proper diagnosis. Symptoms may be dismissed as normal menstrual discomfort. However, recognizing these symptoms early can lead to better treatment options.
Endometriosis management can include medical therapies and surgery. Treatments aim to reduce pain and improve quality of life. Some options include hormonal therapies and laparoscopic surgery to remove visible endometriosis tissue. Surgery can help restore normal anatomy, improving the chances of conception.
Mild endometriosis might respond well to medication alone. More advanced cases may require more invasive procedures like IVF (in vitro fertilization) to achieve pregnancy. Success rates vary based on individual circumstances, such as age and severity of the condition.
Surgical Treatment and Its Impact
Laparoscopic Surgery
Laparoscopic surgery is a common method for treating endometriosis. This minimally invasive technique allows doctors to remove endometrial tissue through small incisions. Many patients experience less pain and quicker recovery times with this approach.
In a speculum exam, doctors can assess the severity of endometriosis. If they suspect significant growth, they may recommend a diagnostic laparoscopy. During this procedure, they can visualize the internal organs and identify scar tissue. Studies show that removing endometriosis can improve fertility outcomes, especially in younger women.
Fertility Outcomes
The extent of endometriosis directly affects future fertility. Women with mild endometriosis may have better chances of conceiving after surgery than those with severe cases. Research indicates that surgical treatment can increase pregnancy rates significantly.
Younger women often benefit most from surgical removal of endometrial lesions. The removal of scar tissue improves the chances of natural conception. For instance, a study published in 2020 found that women who underwent laparoscopic surgery had a 50% higher chance of becoming pregnant within two years compared to those who did not have surgery.
Risks of Surgery
Repeated surgeries carry risks that women should consider. One major concern is ovarian egg loss. Each time a woman undergoes surgery, there is a chance of damaging healthy ovarian tissue. This can lead to decreased egg reserve over time.
Multiple surgeries may cause more scar tissue to form. This can complicate future procedures or even hinder fertility further. A careful evaluation of the benefits and risks is essential before deciding on surgical options.
Time Considerations
Time plays a crucial role in managing endometriosis and improving fertility. Delaying surgical intervention may worsen the condition, making it harder to conceive later on. Women often face challenges when trying to balance treatment decisions with their desire to start a family.
Doctors recommend early intervention for optimal outcomes. They encourage women experiencing symptoms to seek evaluations sooner rather than later. Early diagnosis and timely surgical treatment can make a significant difference in fertility success rates.
Medical Approaches to Infertility
Comprehensive Evaluation
A thorough fertility evaluation is essential before starting any treatment. Doctors assess various infertility factors to identify the root cause. This evaluation often includes blood tests, imaging studies, and a detailed medical history.
Understanding each patient’s unique situation helps tailor the treatment plan. For instance, unexplained infertility can result from multiple factors like hormonal imbalances or anatomical issues. Identifying these conditions early increases the chances of successful fertility treatments.
Stages of Endometriosis
Medical treatments for endometriosis depend on its stage. The stages range from minimal to severe. Early-stage endometriosis may respond well to medication alone. Hormone therapy is commonly used at this stage to manage symptoms and improve fertility.
In contrast, advanced stages often require more aggressive interventions. Fertility treatments may include surgery, such as ovarian cystectomy, to remove endometrial tissue and restore normal anatomy. These surgeries aim to clear blockages and enhance the chances of conception.
Hormonal Therapy’s Role
Hormone therapy plays a critical role in managing endometriosis-related infertility. This treatment regulates hormone levels that can exacerbate symptoms. By controlling these hormones, doctors can reduce pain and improve overall reproductive health.
Common hormone treatments include birth control pills, GnRH agonists, and progestins. Each option works differently but aims to suppress the growth of endometrial tissue. This suppression can lead to less inflammation and fewer pregnancy complications.
Hormonal treatments also help prepare the body for potential pregnancy. They create a more favorable environment for implantation if conception occurs. Patients often see improvements in their menstrual cycle regularity and symptom relief with consistent hormone therapy.
Treating Early Stages with Clomiphene IUI
Clomiphene Overview
Clomiphene is a common first-line treatment for women with Stage I-II endometriosis. This medication helps stimulate ovulation. It works by blocking estrogen receptors in the hypothalamus. This increases the release of hormones that promote ovulation. Many doctors recommend it as an initial approach to enhance fertility.
Understanding IUI
IUI, or intrauterine insemination, is a procedure that can improve the chances of conception. During IUI, a doctor places sperm directly into a woman’s uterus. This timing aligns with ovulation. The goal is to increase the number of sperm that reach the fallopian tubes. This method can be particularly effective when combined with Clomiphene.
The process begins with monitoring ovulation. Doctors often use ultrasound and blood tests to track hormone levels. Once the egg is mature, they perform the IUI procedure. A thin catheter delivers concentrated sperm into the uterus. This minimizes the distance sperm must travel to fertilize an egg.
Next Steps After Treatment
If Clomiphene IUI does not result in pregnancy, several options are available. Doctors may suggest increasing the dosage of Clomiphene or trying another cycle of IUI. It’s also possible to consider additional fertility treatments.
Another option is in vitro fertilization (IVF). IVF involves retrieving eggs from the ovaries and fertilizing them outside the body. This method can bypass some challenges associated with endometriosis.
Women may also explore other medications or hormonal therapies. These alternatives aim to manage endometriosis symptoms while enhancing fertility potential.
Support groups and counseling can help during this journey. Emotional support plays a vital role in coping with infertility challenges.
Approaches for Advanced Stages
IVF Recommendation
In cases of Stage III-IV endometriosis, in vitro fertilization (IVF) often becomes the primary treatment option. Studies show that IVF can significantly improve fertility rates for women with advanced endometriosis. The condition can cause severe damage to the reproductive system. This damage affects the tubes and ovaries, making natural conception difficult.
Many doctors recommend starting IVF after surgical treatment. Surgery may help remove some of the endometrial tissue. However, waiting too long after surgery can decrease the likelihood of success. Most experts suggest considering IVF within six months following surgery. This timeline allows for optimal recovery while still capitalizing on improved fertility potential.
Tailored Strategies
Tailoring fertility strategies is essential for each patient. Factors like age, overall health, and specific symptoms play critical roles in forming a plan. Women over 35 may face higher difficulty levels due to age-related factors. Younger women might have different options available.
Doctors often assess each patient’s unique situation before suggesting a course of action. Some patients may benefit from hormonal treatments to manage symptoms before IVF. Others might need additional tests to evaluate their reproductive system further.
Importance of Timing
Timing plays a crucial role in the effectiveness of fertility treatments. Women should track their menstrual cycles closely. Understanding cycle days can help identify the best times for procedures like IVF or insemination.
Research indicates that early intervention leads to better outcomes. Delaying treatment can lead to more extensive damage from endometriosis, reducing chances of pregnancy later on. Patients should maintain open communication with their healthcare team about any changes in symptoms or concerns.
Emotional Support
Women facing advanced endometriosis often experience emotional challenges. The journey through infertility can be stressful and isolating. Seeking support is vital for mental well-being during this time.
Support groups and counseling services provide valuable resources. Connecting with others who share similar experiences fosters understanding and encouragement. Patients should not hesitate to reach out for help when needed.
In-Vitro Fertilization Techniques
Ovarian Stimulation
Ovarian stimulation is the first step in the IVF process. Doctors use medications to encourage the ovaries to produce multiple eggs. This is crucial because more eggs increase the chances of successful fertilization.
After a few days, doctors monitor egg development using ultrasound. They check how many follicles are growing and their sizes. Once the eggs are ready, a trigger shot of hormones induces ovulation. This usually occurs about 36 hours before egg retrieval.
Egg Retrieval
Egg retrieval occurs through a laparoscopic method. A thin tube goes through the vaginal canal and into the ovaries. This procedure takes about 20 minutes and is done under sedation.
Doctors use ultrasound guidance to locate the follicles filled with eggs. They then suction out the eggs from each follicle. The retrieved eggs are sent to a fertility laboratory for fertilization.
Fertilization Process
Fertilization can happen in two ways: traditional insemination or intracytoplasmic sperm injection (ICSI). In traditional insemination, sperm and eggs are combined in a dish. ICSI involves injecting a single sperm directly into an egg.
This choice depends on factors like sperm quality or previous fertilization issues. The goal is to create viable embryos that can be transferred back into the uterus.
Embryo Quality and Selection
The quality of embryos plays a significant role in pregnancy rates. Not all embryos develop properly after fertilization. Therefore, embryologists assess them based on their appearance and growth patterns.
High-quality embryos have better chances of implantation and leading to pregnancy. Clinics often use genetic testing to select the healthiest embryos for transfer. This increases the likelihood of successful outcomes.
Emotional and Financial Considerations
IVF can be emotionally challenging and financially taxing. Many women experience anxiety during this process due to uncertainty around outcomes. Support from family, friends, or counseling services can help manage these feelings.
Financially, IVF treatments can be expensive. Costs vary widely depending on location and specific treatments needed. Many insurance plans do not cover IVF, which adds to the financial burden for many families.
Understanding these emotional and financial aspects is essential for anyone considering IVF as a treatment option for endometriosis-related fertility issues.
Assisted Reproductive Technologies
ICSI
Intracytoplasmic Sperm Injection (ICSI) is a significant advancement in assisted reproductive technologies. This method involves injecting a single sperm directly into an egg. It helps women with endometriosis who may have issues with sperm penetration. ICSI increases the chances of fertilization, especially when traditional methods fail.
Many clinics report higher success rates with ICSI compared to standard IVF for women facing fertility challenges due to endometriosis. This technique allows doctors to select the healthiest sperm, improving embryo quality. Studies show that using ICSI can lead to better outcomes for women with this condition.
Egg Freezing
Egg freezing offers another innovative option for women with endometriosis. This procedure allows women to preserve their eggs for future use. It provides flexibility for those who may wish to delay pregnancy due to health concerns or personal choices.
Advancements in freezing techniques have improved the survival rates of frozen eggs. Vitrification is a rapid freezing process that enhances egg viability. Women can now plan their families more effectively without the immediate pressure of fertility decline.
Technological Advancements
Recent technological advancements play a crucial role in improving success rates for women with endometriosis. New imaging techniques help doctors monitor embryo development more accurately. Tools like time-lapse imaging allow continuous observation of embryos, leading to better selection for transfer.
Moreover, genetic testing of embryos has become more common. Preimplantation Genetic Testing (PGT) identifies genetic abnormalities before implantation. This ensures that only healthy embryos are transferred, increasing the likelihood of successful pregnancies.
Personalized Treatment Plans
Personalized treatment plans are essential in assisted reproductive technologies. Each woman’s experience with endometriosis is unique. Factors such as age, severity of the condition, and overall health influence treatment options.
Doctors assess these factors when creating tailored plans. They may recommend combining different techniques, such as ICSI and egg freezing, based on individual needs. This personalized approach maximizes the chances of conception and leads to better outcomes.
Women should discuss their specific situations with healthcare providers. Open communication helps ensure that all options are explored and understood.
Additional Supportive Treatments
Lifestyle Modifications
Diet and exercise play a crucial role in managing endometriosis. A balanced diet can help reduce inflammation. Foods rich in omega-3 fatty acids, like fish, may improve overall health. Fruits and vegetables provide essential vitamins that support the immune system.
Maintaining a healthy weight is also important. Excess weight can worsen symptoms and impact fertility. Regular exercise helps improve circulation and reduces stress. Engaging in activities like yoga or walking can be beneficial for both physical and mental health.
Alternative Therapies
Alternative therapies offer additional options for symptom relief. Acupuncture is one such method. Studies show it may help reduce pain associated with endometriosis. This therapy involves inserting thin needles into specific points on the body. Many women report feeling more relaxed after sessions.
Herbal treatments are another alternative. Some herbs may help manage symptoms, but consulting a healthcare provider is essential before starting any new medication or treatment. Combining these therapies with traditional treatments can lead to better outcomes.
Mental Health Support
Mental health support is vital during fertility treatments. The emotional toll of endometriosis can be significant. Stress and anxiety may affect overall well-being and fertility. Seeking counseling or joining support groups can provide relief.
Talking to others who understand the struggles can be comforting. These connections foster a sense of community and shared experience. Mental health professionals can offer coping strategies to manage stress effectively.
Partner Involvement
The involvement of a partner is crucial in navigating this journey. Open communication strengthens relationships during challenging times. Partners can attend appointments, providing emotional support. They can also participate in lifestyle changes together, promoting a healthier environment for both individuals.
Importance of Testing
Regular testing is essential for monitoring endometriosis progression. Routine examinations, including pap tests, help assess reproductive health. These tests check for abnormalities that could affect fertility.
Early detection of cysts or other issues allows for timely intervention. Staying informed about one’s health empowers individuals to make better decisions regarding treatment options.
Summary
Navigating endometriosis and its impact on fertility can be overwhelming. You’ve explored various innovative treatments, from surgical options to advanced reproductive technologies. Each approach offers unique benefits tailored to your specific needs. Understanding these treatments empowers you to make informed decisions about your fertility journey.
Take charge of your health today. Consult with a specialist to discuss which treatments suit you best. The right support can significantly enhance your chances of conception. Don’t hesitate to seek guidance and explore these innovative options. Your path to parenthood is within reach, and every step counts.
Frequently Asked Questions
What is endometriosis and how does it affect fertility?
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus. This can cause inflammation, pain, and scarring, which may hinder fertility by blocking fallopian tubes or disrupting hormonal balance.
What surgical options are available for treating endometriosis?
Surgical treatments include laparoscopic excision or ablation of endometrial tissue. These procedures can relieve symptoms and improve fertility by removing lesions and adhesions, allowing for better reproductive function.
How do medical treatments help with infertility caused by endometriosis?
Medical treatments like hormonal therapy aim to reduce or eliminate endometriosis lesions. By managing symptoms and regulating hormones, these therapies can enhance the chances of conception and improve overall fertility.
Can Clomiphene citrate and IUI be effective for early-stage endometriosis?
Yes, Clomiphene citrate combined with intrauterine insemination (IUI) is often effective for women with early-stage endometriosis. This approach stimulates ovulation and increases the likelihood of sperm meeting the egg.
What advanced treatment options are available for severe endometriosis?
For advanced stages, options include more extensive surgery or assisted reproductive technologies (ART) like in-vitro fertilization (IVF). These methods address both the physical barriers to conception and optimize reproductive outcomes.
How does in-vitro fertilization (IVF) work for women with endometriosis?
IVF involves retrieving eggs from the ovaries, fertilizing them in a lab, and implanting embryos into the uterus. This bypasses many complications of endometriosis, increasing the likelihood of pregnancy.
Are there supportive treatments that can enhance fertility in women with endometriosis?
Yes, supportive treatments such as acupuncture, dietary changes, and stress management techniques can complement medical interventions. These approaches may improve overall health and create a more favorable environment for conception.
