Posted September 21, 2024 in Fertility Blog & Information
17 minute read
Endometriosis and fertility management can feel like a tough battle. Many women face the pain of endometriosis and endometrioma while dreaming of starting a family and considering fertility treatment. It’s a harsh contrast—pain versus hope. Understanding how endometriosis impacts fertility is crucial for those navigating this journey.
Managing symptoms and exploring treatment options can open doors to better chances of conception. This blog dives into practical strategies, expert insights, and real-life experiences related to mild endometriosis to empower you. Whether you’re just beginning to learn about endometriosis or seeking ways to improve your fertility, we’ve got you covered. Let’s break down the barriers together and shed light on effective management techniques that can help turn dreams into reality.
Key Takeaways
- Understand that endometriosis can significantly affect fertility, so early diagnosis is crucial for managing reproductive health.
- Seek a specialist for accurate diagnosis and explore various medical treatments that can help improve fertility outcomes.
- Consider surgical options if medical treatments are not effective, as they may help alleviate symptoms and enhance fertility chances.
- For those in the early stages, Clomiphene and IUI can be effective methods to boost ovulation and increase the likelihood of conception.
- If endometriosis is advanced, discuss In-Vitro Fertilization (IVF) with your healthcare provider as a viable option for achieving pregnancy.
- Stay informed about assisted reproductive techniques, as they offer additional pathways to parenthood for those facing fertility challenges due to endometriosis.
Understanding Endometriosis and Fertility
Definition
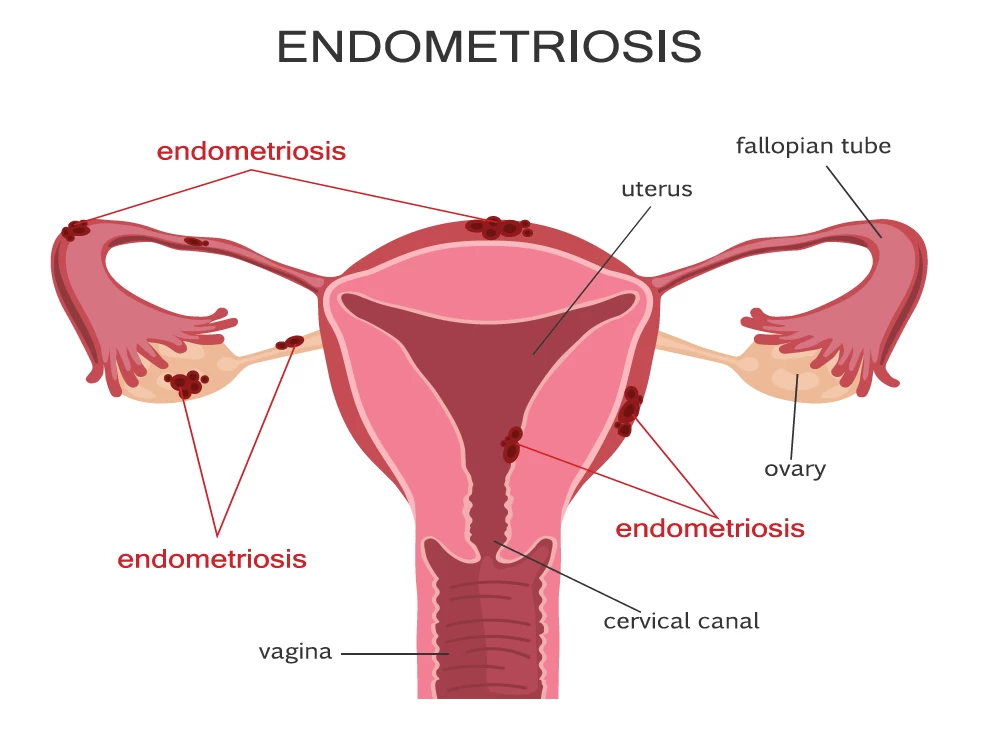
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus. This can cause pain and other complications. It affects about 1 in 10 women of reproductive age. Symptoms often include severe menstrual cramps, chronic pain, and heavy periods.
Impact on Fertility
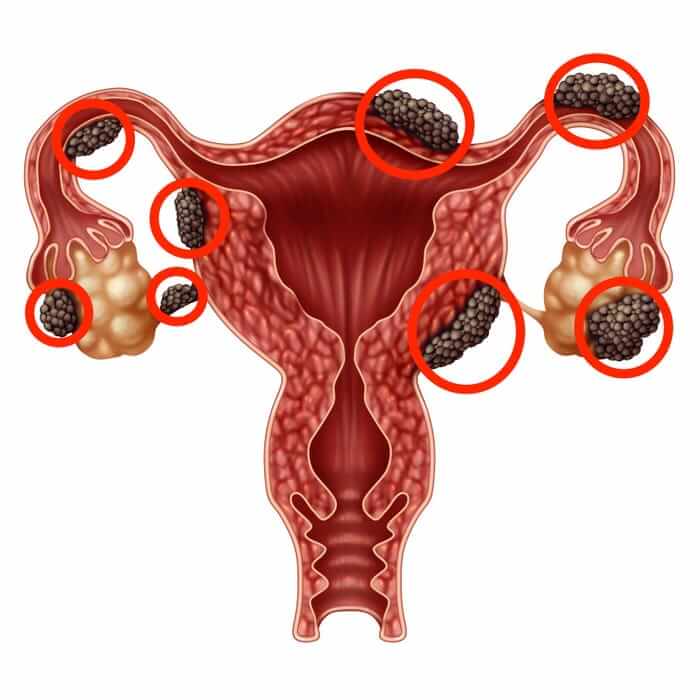
Endometriosis can significantly inhibit ovulation. The presence of endometrial-like tissue can disrupt the normal functioning of ovaries. It may lead to the formation of cysts and scar tissue, which impacts the development of follicles. These follicles are essential for releasing eggs during ovulation.
Women with endometriosis may face challenges in conceiving. The condition can result in blocked fallopian tubes or changes in hormone levels. These factors can complicate the fertilization process. Research indicates that women with endometriosis may have a lower fertility rate compared to those without the condition.
Importance of Early Diagnosis
Early diagnosis plays a crucial role in managing fertility issues related to endometriosis. Identifying the condition early allows for timely treatment options. Treatments may include medication or surgery to remove endometrial tissue.
The earlier a woman seeks help, the better her chances of successful fertility management. Regular check-ups and discussions with healthcare providers are vital. These steps ensure that any symptoms are not overlooked.
In the UK, awareness about endometriosis is growing. Many organizations provide resources for women experiencing symptoms. They emphasize the need for education about this condition and its effects on fertility.
Treatment Options
Several treatment options exist for managing endometriosis and enhancing fertility. Hormonal therapies aim to reduce or eliminate menstruation, which can lessen symptoms. Surgical options may involve laparoscopic procedures to remove lesions.
Lifestyle changes also play a role in managing symptoms. Maintaining a healthy diet and regular exercise can improve overall well-being. Stress management techniques, such as yoga or meditation, may offer additional support.
Support Systems
Support systems are important for women dealing with endometriosis and fertility challenges. Connecting with others who share similar experiences can be beneficial. Online forums and local support groups provide spaces for sharing information and emotional support.
Diagnosing Endometriosis for Fertility Issues
Diagnostic Methods
Various methods exist for diagnosing endometriosis. Pelvic exams play an essential role. During this exam, a doctor checks for abnormalities in the pelvic region. A speculum exam is often performed to visualize the vagina and cervix. This helps identify any unusual growths or lesions.
Ultrasounds are also common. They can reveal cysts linked to endometriosis. However, ultrasounds cannot definitively diagnose the condition. Many women with endometriosis may have normal ultrasound results.
Laparoscopy Confirmation
Laparoscopy is crucial for confirming an endometriosis diagnosis. This minimally invasive surgery allows doctors to view the pelvic organs directly. A camera is inserted through small incisions in the abdomen. If endometrial tissue is found outside the uterus, it confirms the diagnosis.
This procedure also allows for treatment options. Doctors can remove abnormal tissue during laparoscopy. It provides immediate relief and helps improve fertility chances.
Importance of Fertility Evaluation
A comprehensive fertility evaluation is vital before starting treatment. This evaluation assesses overall reproductive health. It includes tests like hormone level checks and sperm analysis for partners.
Understanding endometriosis-associated infertility is important. The condition can affect fertility in various ways. Blocked fallopian tubes or hormonal imbalances may occur due to endometriosis.
The Endometriosis Fertility Index (EFI) helps evaluate a woman’s chance of conceiving. It considers factors like age, previous pregnancies, and severity of endometriosis. This index guides doctors in tailoring treatment plans.
Asymptomatic Endometriosis
e women experience asymptomatic endometriosis. They may not show symptoms but still face fertility challenges. Regular check-ups become crucial for these women. Early detection can lead to better management strategies.
Induced endometriosis is another concern. This occurs when endometrial-like tissue forms due to surgeries or hormonal treatments. Recognizing its impact on fertility is essential for effective management.
Effects of Endometriosis on Reproductive Health
Anatomical Changes
Endometriosis can lead to significant anatomical changes in the reproductive system. The growth of endometrial tissue outside the uterus can form adhesions and scar tissue. These changes may obstruct fallopian tubes or distort the shape of the uterus.
Such alterations can hinder the movement of eggs from the ovaries to the uterus. They can also affect sperm transport, making it difficult for fertilization to occur. These anatomical issues often result in infertility or challenges in conceiving.
Inflammation and Hormonal Imbalances
Inflammation plays a crucial role in the impact of endometriosis on fertility. The presence of endometrial tissue outside the uterus can trigger an inflammatory response. This inflammation can create a hostile environment for sperm and eggs.
Hormonal imbalances are another significant factor. Endometriosis disrupts normal hormonal cycles, affecting ovulation and menstrual regularity. Irregular ovulation reduces the chances of conception. Hormones like estrogen can promote the growth of endometrial tissue, worsening symptoms and further complicating fertility management.
Psychological Effects
The psychological effects of endometriosis on women trying to conceive are profound. Many experience anxiety and depression due to ongoing pain and uncertainty about their reproductive health. The struggle with infertility adds another layer of emotional distress.
Women may feel isolated or misunderstood by friends and family who do not share similar experiences. This emotional burden can lead to feelings of inadequacy or low self-esteem. Seeking support from mental health professionals or support groups can be beneficial for coping with these feelings.
Medical Treatments for Infertility
Treatment Options
Doctors offer various fertility treatments based on the stage of endometriosis. The stages are classified from I (minimal) to IV (severe).
For stage I and II, treatment may include medications like non-steroidal anti-inflammatory drugs (NSAIDs) to manage pain. Hormonal therapies are often prescribed to reduce the growth of endometrial tissue. These treatments can help improve fertility by creating a more favorable environment for conception.
In stage III and IV, doctors might recommend more aggressive interventions. Fertility treatments such as in vitro fertilization (IVF) become options. IVF bypasses many issues related to endometriosis by directly fertilizing eggs outside the body. This method has shown success rates for women with severe endometriosis.
Hormonal Therapies
Hormonal therapies play a crucial role in managing symptoms of endometriosis. Medications such as birth control pills, progestins, and GnRH agonists help regulate hormone levels. These medications work by suppressing menstruation and reducing the growth of endometrial tissue.
The use of hormonal therapy not only alleviates pain but also improves fertility outcomes. For example, GnRH agonists can create a temporary menopause-like state. This reduces inflammation and may enhance the chances of pregnancy once hormone levels return to normal.
Personalized Treatment Plans
Personalized treatment plans are vital for effective management of infertility due to endometriosis. Each woman’s experience with the condition is unique. Factors such as age, severity of endometriosis, and overall health influence treatment choices.
A doctor will assess individual circumstances before recommending specific fertility treatments. This tailored approach ensures that women receive the most suitable care based on their needs. Regular monitoring and adjustments may be necessary throughout the treatment process.
Surgical Approaches to Improve Fertility
Types of Procedures
Surgical treatment for endometriosis includes several options. Laparoscopy is the most common procedure. Surgeons use a small camera to view the pelvic organs through tiny incisions. This method allows for the removal of endometrial tissue without large cuts.
Another option is laparotomy. This is a more invasive surgery that involves a larger incision in the abdomen. It may be necessary for severe cases of endometriosis. Surgeons can remove larger cysts or lesions during this procedure.
e patients may benefit from ovarian drilling. This technique uses laser or electrosurgery to destroy tissue on the ovaries. It can help restore normal ovulation and improve fertility chances.
Benefits of Surgery
Surgery can enhance pregnancy rates for many women with endometriosis. Removing endometrial tissue can reduce pain and improve reproductive function. Studies show that women who undergo surgery often experience higher pregnancy rates than those who do not.
For example, a study published in 2021 found that women who had laparoscopic surgery achieved pregnancy within six months at a rate of 60%. In contrast, those who received only medical treatments had lower success rates.
Surgery also helps clear blockages in the fallopian tubes. This is vital since blockages can prevent sperm from reaching the egg. By addressing these issues, surgery increases the likelihood of natural conception.
Considerations for Timing
Timing is crucial when considering surgery for endometriosis. Age plays an important role in decision-making. Younger women may opt for surgery sooner to maximize their fertility window.
The stage of endometriosis matters. Women with mild to moderate cases may benefit more from surgical intervention compared to those with advanced stages. Advanced cases often require a combination of surgical treatment and assisted reproductive technologies like IVF.
Healthcare providers recommend discussing individual situations before deciding on surgery. They can evaluate factors such as age, overall health, and specific symptoms. This personalized approach helps ensure optimal outcomes.
Women should also consider their family planning goals. If they wish to conceive soon, timely surgical intervention might be necessary. However, some may prefer to wait and explore other options first.
Managing Early Stages with Clomiphene IUI
Clomiphene Overview
Clomiphene citrate is a medication often used to treat infertility. It stimulates the ovaries to produce eggs. This drug works by blocking estrogen receptors in the hypothalamus. When this happens, the body thinks estrogen levels are low. As a result, it increases the release of hormones that stimulate ovulation.
Women typically take Clomiphene for five days at the beginning of their menstrual cycle. This treatment can lead to multiple eggs being released during ovulation. For women with early-stage endometriosis, this can be crucial. More eggs increase the chances of conception.
Role of IUI
Intrauterine insemination (IUI) plays a significant role in fertility management for women with endometriosis. During IUI, sperm is placed directly into the uterus around the time of ovulation. This procedure bypasses some barriers that may affect fertility. For women experiencing pain or complications due to endometriosis, IUI offers a less invasive option compared to other methods.
IUI is often combined with Clomiphene treatment. The idea is to enhance the chances of pregnancy when ovulation occurs after taking Clomiphene. By using IUI, healthcare providers aim to increase the likelihood of successful fertilization.
Success Rates
The success rates of combining Clomiphene and IUI vary based on several factors. Age and overall health play a significant role in determining outcomes. Studies show that the success rate for this combination can range from 10% to 20% per cycle for women under 35 years old. For those aged 35 to 40, success rates may drop to around 5% to 15%.
Multiple cycles of Clomiphene and IUI may improve outcomes. Many clinics recommend trying this approach for up to three to six cycles before considering other options. The goal is to maximize the chances of conception while monitoring for any changes in endometriosis symptoms.
Healthcare providers often assess individual cases carefully. They consider factors like ovarian reserve and the severity of endometriosis when recommending treatment plans.
Combining Clomiphene with IUI provides a hopeful pathway for many women facing fertility challenges due to endometriosis. With proper management and support, they can navigate their journey toward motherhood more effectively.
Handling Advanced Stages of Endometriosis
Implications on Fertility
Advanced endometriosis, particularly stage IV endometriosis, significantly affects fertility. In this stage, the tissue grows deeply into organs like the ovaries and bowel. This can lead to scarring and adhesions that disrupt normal reproductive function. Women may experience severe endometriosis pain, making conception difficult.
Moderate to severe endometriosis can also lead to complications such as endometriotic cysts. These cysts can form on the ovaries, impacting egg quality and quantity. The presence of these cysts often complicates natural conception efforts.
Necessity of Aggressive Treatments
For women with untreated endometriosis in advanced stages, more aggressive treatments are often necessary. In vitro fertilization (IVF) becomes a common recommendation. IVF bypasses some of the issues caused by scar tissue and other physical barriers. It allows for direct retrieval of eggs and fertilization outside the body.
Studies show that IVF success rates can be lower in women with severe endometriosis. However, many women still achieve pregnancy through this method. Consulting with an endometriosis specialist is crucial for tailored treatment plans.
Surgery may also be an option for advanced cases. Endometriosis surgery can remove deep endometriosis and adhesions, improving chances of conception. Many specialists recommend a combination of surgery followed by IVF for optimal results.
Importance of Ongoing Monitoring
Women managing advanced stages of endometriosis need ongoing monitoring and support. Regular check-ups help track changes in symptoms and fertility status. This is essential because conditions can evolve over time.
Support groups or counseling can provide emotional relief. Dealing with severe endometriosis pain and infertility can be overwhelming. Connecting with others who share similar experiences can foster understanding and encouragement.
Monitoring also helps address any new complications that arise from bowel endometriosis or other forms of visible endometriosis. Early detection allows for prompt intervention, which can improve overall health outcomes.
In-Vitro Fertilization as a Solution
IVF Process
The in-vitro fertilization (IVF) process involves several steps. First, doctors stimulate the ovaries using hormones. This helps produce multiple eggs instead of the usual one. Next, they retrieve these eggs through a thin tube inserted into the ovaries.
After egg retrieval, sperm is introduced to the eggs in a fertility laboratory. This is where fertilization occurs. The embryos develop for several days before doctors select the best ones for transfer. This method offers women with severe endometriosis a chance to conceive when other treatments fail.
Success Rates
Studies show that IVF can lead to higher pregnancy rates for women with endometriosis compared to natural conception. In cases of moderate to severe endometriosis, the likelihood of becoming pregnant naturally decreases significantly over time. Research indicates that IVF can improve these chances considerably.
For instance, one study found that women with severe endometriosis had a pregnancy rate of about 40% per cycle with IVF. In contrast, natural conception rates were often below 10%. Evidence supports that IVF bypasses some barriers caused by endometriosis, such as damaged fallopian tubes or poor egg quality.
Counseling and Support
Emotional support plays a crucial role during the IVF journey. Couples often face stress and anxiety throughout this process. Counseling can help manage these feelings and provide coping strategies.
Support groups also offer valuable insights from those who have gone through similar experiences. Sharing stories can create a sense of community and reduce feelings of isolation. Couples should seek out resources available in their area or online.
Counseling may also address concerns regarding potential timeframes and financial implications of IVF treatment. Understanding what to expect can ease worries and help couples make informed decisions about their paths to parenthood.
Assisted Reproductive Techniques Overview
Overview of Techniques
Assisted reproductive technologies (ART) include various methods to help individuals conceive. Common techniques are In-Vitro Fertilization (IVF), Intracytoplasmic Sperm Injection (ICSI), and Egg Donation. IVF involves retrieving eggs, fertilizing them in a lab, and transferring embryos back into the uterus. ICSI is a specialized form of IVF where a single sperm is injected directly into an egg. This method can be beneficial for couples with male fertility issues.
Surrogacy is another option for those unable to carry a pregnancy. In this case, another woman carries the baby for the intended parents. Preimplantation Genetic Testing (PGT) can also be used during IVF to screen embryos for genetic conditions before implantation. Each technique has its own success rates and risks.
Selecting Appropriate Techniques
Choosing the right ART depends on several factors. Age plays a crucial role, as younger women generally have higher success rates with ART. The severity of endometriosis impacts options available. Women with mild endometriosis may respond well to standard IVF, while those with severe cases might need more advanced techniques like ICSI or donor eggs.
Health history also influences decisions. Previous surgeries, hormone levels, and ovarian reserve tests provide insights into the best approach. Consulting with a fertility specialist helps clarify these options. They can offer personalized recommendations based on individual circumstances.
Multidisciplinary Approach Importance
Managing fertility challenges linked to endometriosis requires a multidisciplinary approach. This means involving various healthcare professionals in treatment planning. Gynecologists, reproductive endocrinologists, and nutritionists all play essential roles.
Each professional brings unique expertise to the table. Gynecologists focus on treating endometriosis symptoms and improving reproductive health. Reproductive endocrinologists specialize in ART and hormonal treatments. Nutritionists can guide dietary changes that support overall health and fertility.
Closing Thoughts
Navigating endometriosis and fertility can feel overwhelming, but you’re not alone. Understanding how this condition affects your reproductive health is key. From diagnosis to treatment options, each step you take brings you closer to managing your fertility effectively. Whether it’s medical treatments or surgical options, knowing what’s out there empowers you to make informed choices.
Take charge of your journey. Connect with healthcare professionals who understand your needs and explore all available resources. You deserve support and guidance as you tackle these challenges head-on. Remember, every step counts in this journey towards achieving your dreams of parenthood. So, gather your questions, seek answers, and don’t hesitate to reach out for help. You’ve got this!
Frequently Asked Questions
What is endometriosis, and how does it affect fertility?
Endometriosis occurs when tissue similar to the lining of the uterus grows outside it. This can cause inflammation, scarring, and pain, making it harder to conceive.
How is endometriosis diagnosed in relation to fertility issues?
Doctors typically use pelvic exams, ultrasounds, and laparoscopy to diagnose endometriosis. These methods help identify the location and extent of the tissue growth affecting fertility.
Can endometriosis impact my chances of getting pregnant?
Yes, endometriosis can lead to infertility. It may block fallopian tubes or disrupt hormonal balance, making conception more challenging.
What medical treatments are available for infertility caused by endometriosis?
Treatment options include hormonal therapies like birth control pills or GnRH agonists. These can help manage symptoms and improve your chances of conception.
When should I consider surgical options for endometriosis?
If other treatments fail or if you have severe symptoms, surgery might be necessary. It can remove endometrial tissue and adhesions, potentially enhancing fertility.
How does Clomiphene IUI work for early-stage endometriosis?
Clomiphene citrate stimulates ovulation, while intrauterine insemination (IUI) places sperm directly in the uterus. This combination can increase your chances of pregnancy in early-stage endometriosis.
Is In-Vitro Fertilization (IVF) a viable option for advanced endometriosis?
Absolutely! IVF bypasses many complications of natural conception. It allows for direct fertilization and embryo transfer, making it an effective solution for advanced cases.
