Blog
- CATEGORIES:
-
Why You Should Freeze Your Eggs Before Age 35

Many women are choosing to take control of their fertility journey — sometimes years before they are ready to conceive. Future fertility planning comes in many forms, and one of […]
What Is Egg Freezing?

Fertility planning looks different for everyone. Some parents start their paths as soon as possible, while others start their journey by planning for the future. If your fertility plan involves […]
7 Reasons to Consider Gestational Surrogacy

3 Minute Read: Countless couples and individual parents have successfully started their families using a gestational surrogate, beginning their journey to parenthood. 1. Overcoming Infertility Many intended parents who choose […]
Understanding IVF: Is It Right for Your Fertility Journey

3 Minute Read: Deciding to have a baby is exciting, but if conception is proving difficult, things can quickly become frustrating. When faced with infertility or difficulty conceiving, many people […]
Donor Egg IVF: What You Need to Know

4 Minute Read: There are many paths to fertility. With so many options available, it is important for you to consider what is important for you and your family during […]
What to Expect Before, During, and After an IUI Procedure

Infertility is a lot more common than many people think, with 9% and 11% of men and women respectively reporting difficulty getting pregnant. However, people in this situation aren’t without the […]
How Long Is the Process of IVF?

Are you experiencing difficulty having a child? If so, you’re not alone. Reports show that up to one in seven couples struggle to become pregnant. In America, 33 percent of people have […]
What Is Polycystic Ovary Syndrome (PCOS)? It’s Not Just Infertility

Do you sometimes go two to three months without having a menstrual cycle or does it come far sooner than you expected? Are your cycles extremely heavy, and do you […]
When can I get the Covid-19 Vaccine?

The approval of the Pfizer and Moderna vaccines has been a major step forward in fighting Coronavirus. Now the main question seems to be: When will I be able to […]
How Can a Same Sex Female Couple Have a Baby? The Ultimate Guide

Getting married and having children is something many of us look forward to from the time we ourselves are children. We play with baby dolls and cuddle relatives’ babies, dreaming […]
What is Intracytoplasmic Sperm Injection (ICSI)?
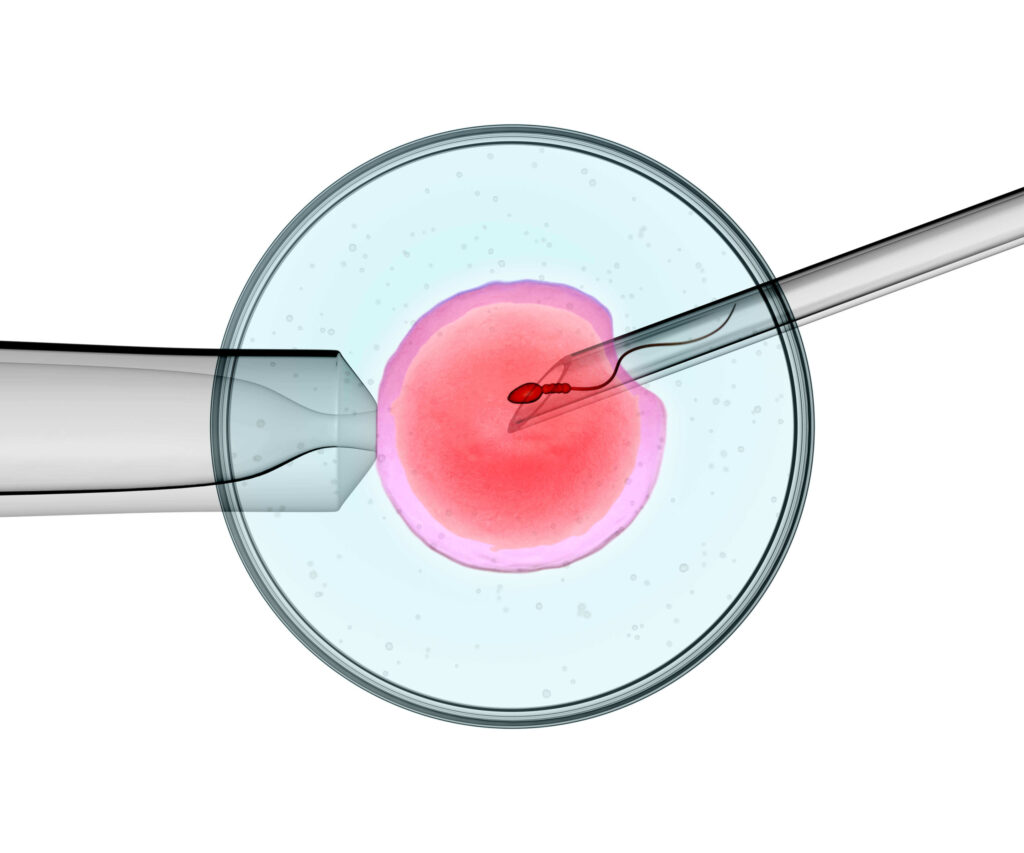
Getting pregnant can be more challenging than it seems, with recent studies suggesting that about 1 in every 5 women have difficulty conceiving Before a sperm can fertilize an egg, […]
