Posted March 08, 2025 in Fertility Blog & Information
18 minute read
Understanding IVF success rates is crucial for anyone considering this infertility treatment path to parenthood, especially when facing fertility problems and exploring efficient fertility practices like intrauterine insemination. These rates can vary widely based on several factors, including age, health, clinic expertise, cost, number, result, and birth. Knowing the numbers helps set realistic expectations.
Many couples feel overwhelmed by the choices ahead. With the right information, you can make informed decisions about baby fertilisation rates that align with your prior IVF goals. This post dives into what affects IVF success rates and how to improve your chances of having a baby. Get ready to explore essential insights that can guide your rate journey toward starting a family.
Key Takeaways
- Understanding IVF: Familiarize yourself with the IVF process, its components, and success rate to make informed decisions about your fertility journey.
- Age Matters: Be aware that IVF success rates vary significantly by age, so consider this when planning your treatment.
- Consult Your GP: Discuss your options and concerns with your general practitioner to get personalized advice, rate your needs, and referrals to specialists.
- Evaluate Factors: Rate the various factors affecting IVF success, such as health conditions and lifestyle choices, to enhance your chances.
- Choose Wisely: Select a fertility team with a good track record and rate of expertise in IVF to ensure you receive the best possible care.
- Implement Tips: Follow practical tips to improve your IVF success, such as maintaining a healthy lifestyle and managing stress levels.
What is IVF
Definition
IVF stands for In Vitro Fertilization. It is a medical procedure that helps couples conceive. The process involves fertilizing an egg with sperm outside the body. This occurs in a controlled laboratory environment.
Process Overview
The first step in IVF is ovarian stimulation. Doctors use medications to stimulate the ovaries to produce multiple eggs. This increases the chances of successful fertilization. After about 10-14 days, doctors retrieve the eggs using a minor surgical procedure.
Next, eggs are combined with sperm in a laboratory dish. This creates embryos through fertilization. The lab monitors these embryos for several days. Usually, they observe them for 3 to 5 days until they reach the blastocyst stage.
Embryo Transfer
Once embryos are ready, doctors transfer them into the uterus. This usually happens during a simple outpatient procedure. A thin tube called a catheter delivers the embryos into the uterus. The goal is to achieve pregnancy by allowing the embryo to implant in the uterine lining.
Success Factors
Several factors affect IVF success rates. Age plays a crucial role. Younger women generally have higher success rates compared to older women. Health conditions also matter. Conditions like polycystic ovary syndrome (PCOS) or endometriosis can impact outcomes.
Embryo quality influences success as well. High-quality embryos have better chances of implantation and pregnancy. The number of embryos transferred can affect results. Transferring more than one embryo may increase the likelihood of pregnancy but also raises the risk of multiples.
Emotional Aspects
IVF can be an emotional journey for couples. The process often involves hope and anxiety. Many couples feel pressure due to financial costs and time commitments. Support from family and friends can help ease this stress.
Counseling may also benefit couples undergoing IVF. Professional support provides coping strategies and emotional guidance throughout the process.
Who Can Have IVF
Infertility Issues
IVF is a viable option for couples dealing with infertility. Many factors contribute to infertility, including age, health conditions, and lifestyle choices. Couples who have tried other methods without success often turn to IVF. This process can help them achieve their dream of having a child.
Blocked Fallopian Tubes
Women with blocked or damaged fallopian tubes may find IVF particularly beneficial. In natural conception, the fallopian tubes play a crucial role in fertilization. If these tubes are blocked, sperm cannot reach the egg. IVF bypasses this problem by allowing fertilization to occur outside the body. Once fertilized, the embryo is placed directly into the uterus. This method increases the chances of pregnancy for women facing such challenges.
Same-Sex Couples
Same-sex couples also explore IVF as an option for starting a family. They can use donor sperm or eggs to conceive. This process allows them to experience pregnancy and childbirth together. Many clinics offer tailored services for same-sex couples, ensuring they receive comprehensive support throughout the journey.
Single Women
Single women seeking parenthood often consider IVF as well. With advancements in reproductive technology, they can use donor sperm to achieve pregnancy. This option provides single women with more control over their reproductive choices. It empowers them to create families on their own terms.
Age Considerations
Age plays a significant role in fertility and IVF success rates. Women under 35 generally have higher success rates compared to older women. As women age, the quality and quantity of their eggs decline. This decline can affect IVF outcomes. Therefore, younger women may find it easier to conceive through this method.
Health Factors
Certain health conditions can impact fertility and influence the decision to pursue IVF. Conditions like polycystic ovary syndrome (PCOS) or endometriosis may complicate natural conception. IVF offers solutions for these individuals by providing targeted treatments based on their specific needs.
Emotional Support
The journey through IVF can be emotionally challenging. Couples and individuals must navigate various feelings during this process. Emotional support from friends, family, or counseling services is crucial. Many clinics also provide resources to help manage stress and anxiety associated with fertility treatments.
Discussing IVF with Your GP
Scheduling a Consultation
Schedule a consultation with your GP if you have fertility concerns. This meeting is important for understanding your options. A GP can help guide you through the process of IVF. They can also refer you to IVF experts for specialized care.
During this consultation, discuss your medical history. Mention any previous pregnancies or health issues related to your ovaries and womb. This information helps your doctor assess your situation better.
Preliminary Tests
Ask your GP about preliminary tests before starting IVF. Tests usually include blood work and imaging studies. Blood tests check hormone levels and overall health. Imaging studies can evaluate the condition of your eggs and reproductive organs.
These evaluations provide vital information. They help determine the best approach for IVF treatment. Being informed about your body can improve your chances of success.
Costs and Insurance Coverage
Discuss potential costs associated with IVF during your appointment. IVF can be expensive, and knowing the financial aspect is crucial. Ask about the average costs in your area and what they cover.
Inquire about insurance coverage for IVF treatment as well. Some insurance plans provide partial or full coverage for fertility treatments. Understanding your coverage can significantly impact your decision-making process.
Emotional Support
Consider discussing emotional support options with your GP. Fertility treatments can be stressful for many women. Having a support system is essential during this time. Your GP may recommend counseling services or support groups.
Being prepared emotionally can enhance your overall experience with IVF. It allows you to focus on the journey ahead.
Next Steps
After consulting with your GP, take note of the next steps. Follow up on any recommended tests promptly. This proactive approach shows commitment to your fertility journey.
Stay informed about all aspects of the process as well. Reading reliable resources about IVF can help you understand what to expect.
What Happens During IVF
Ovarian Stimulation
The usual IVF procedure begins with ovarian stimulation. This step is crucial for producing multiple eggs. Doctors prescribe hormone injections to stimulate the ovaries. These hormones help the ovaries grow several follicles, each containing an egg.
Monitoring occurs through blood tests and ultrasounds. This process helps track follicle growth and hormone levels. Typically, this phase lasts about 10 to 14 days. The goal is to gather as many viable eggs as possible.
Egg Retrieval
Once the follicles reach maturity, egg retrieval follows. This procedure occurs under sedation to ensure comfort. A doctor uses a thin needle guided by ultrasound to extract the eggs from the ovaries.
The process takes about 20 minutes. Patients usually go home shortly after recovery. Some experience mild cramping or discomfort, but serious complications are rare.
Fertilisation Process
After egg retrieval, fertilisation takes place in a laboratory setting. The collected eggs are combined with sperm from a partner or donor. This can happen through various methods, including artificial insemination or direct injection of sperm into the egg.
Successful fertilisation results in embryos. These embryos are cultured for several days in a controlled environment. During this time, they develop and grow.
Doctors typically monitor the embryos for quality and development. By day five, some embryos reach the blastocyst stage, which is ideal for transfer.
Embryo Transfer
The final step involves transferring one or more healthy embryos into the uterus. This occurs through a simple procedure using a thin catheter. It requires no anesthesia and usually takes only a few minutes.
Doctors may recommend transferring multiple embryos to increase success rates. However, this decision depends on individual circumstances and previous outcomes like prior IVF attempts.
Following the transfer, patients may wait about two weeks before taking a pregnancy test. This period can be filled with anxiety and hope.
Factors Affecting IVF Success
Age Impact
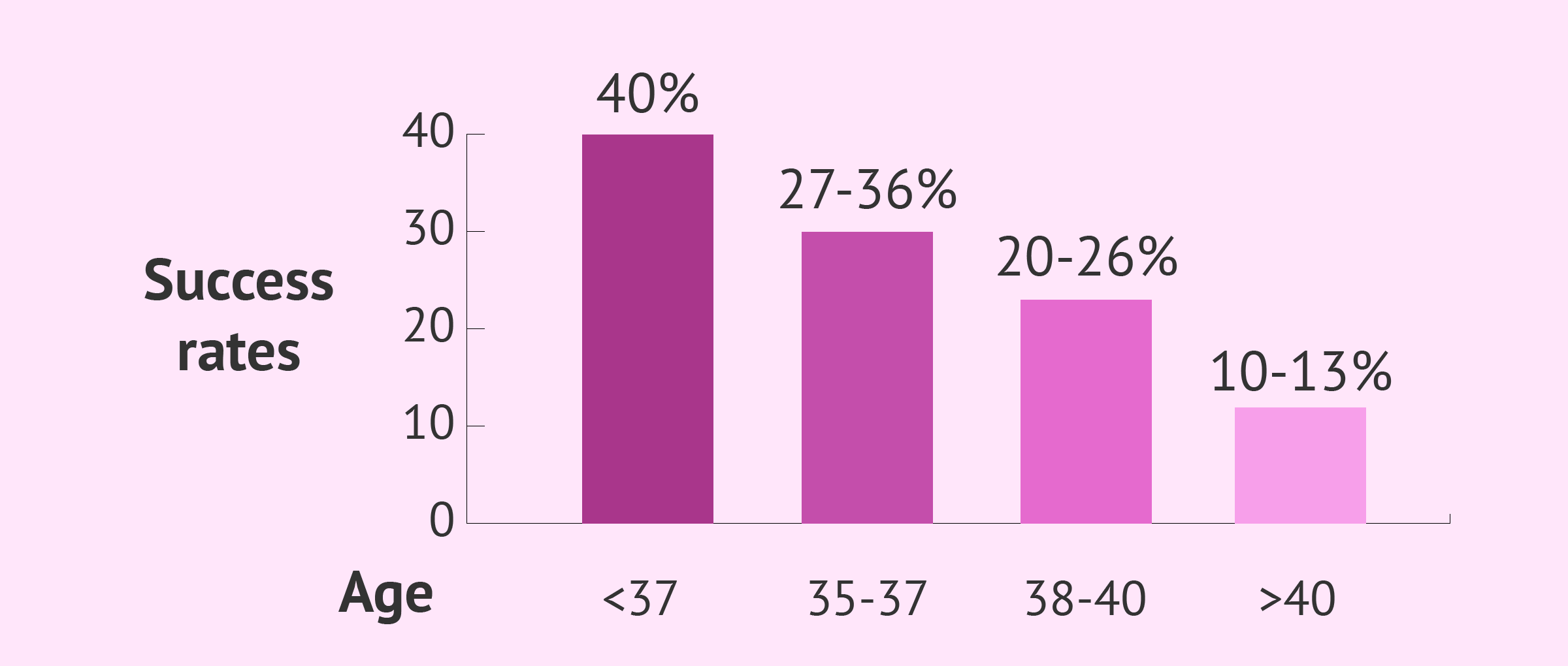
A woman’s age plays a crucial role in the success of IVF. Younger women typically have higher success rates. For instance, women under 35 have about a 40% chance of success per cycle. As women age, especially after 35, this rate declines significantly. By age 40, the success rate drops to around 15%.
This decline occurs because egg quality decreases with age. Older eggs are more likely to have chromosomal abnormalities. These issues can lead to unsuccessful IVF attempts. Therefore, age is one of the most critical factors affecting IVF outcomes.
Infertility Causes
The cause of infertility also impacts IVF success. Different conditions affect the chances differently. Women with unexplained infertility may have similar success rates as those with known issues. However, specific causes like endometriosis or severe male factor infertility can lower the odds.
For example, women with endometriosis face challenges that may hinder embryo implantation. Similarly, men with low sperm counts may struggle to produce viable embryos. Understanding these causes helps tailor treatment plans for better results.
Lifestyle Choices
Lifestyle factors significantly influence IVF success rates. Weight is a key factor; both underweight and overweight women face challenges. Obesity can lead to hormonal imbalances, impacting egg production and embryo quality. Maintaining a healthy weight can improve outcomes.
Smoking has detrimental effects on fertility as well. It reduces ovarian function and can harm embryos during development. Studies show that women who smoke have lower success rates compared to non-smokers. Quitting smoking before starting IVF can enhance chances of conception.
Alcohol consumption also affects fertility and IVF success rates. Heavy drinking can disrupt hormone levels and reduce egg quality. Women are advised to limit or eliminate alcohol intake when undergoing IVF treatment.
Emotional Considerations
Emotional health is another important factor in IVF success. Stress can negatively impact fertility treatments. High-stress levels may interfere with hormone balance, affecting the body’s response to IVF medications.
Many couples find support through counseling or support groups during this process. Open communication between partners can also help manage stress levels effectively.
IVF Success Rates by Age
Age Factors
Success rates for IVF vary significantly based on a woman’s age. For women under 35, the success rate is approximately 32%. This means that about one-third of women in this age group achieve pregnancy per embryo transferred.
As women age, these rates decline. Women aged 35 to 37 see a success rate drop to around 26%. The numbers continue to decrease for those aged 38 to 40, where the success rate falls to about 20%.
Older Women
The decline becomes more pronounced for women over 42. In this group, the success rates can drop to as low as 5% per embryo transferred. This significant decrease highlights the challenges older women face when using their own eggs.
These statistics reflect the biological realities of aging. Factors such as egg quality and uterine health play critical roles in these outcomes.
Method of Calculation
These success rates are based on data from clinics that report outcomes for patients using their own eggs and their partner’s sperm. The statistics consider each embryo transferred during the IVF cycle.
It’s important to note that individual experiences may vary. Some women may have higher or lower chances based on specific medical conditions or treatments received.
Implications of Age
Age impacts not only success rates but also emotional and financial aspects of IVF treatment. Younger women may feel more hopeful due to higher odds of success. Older women might face greater stress and anxiety about their options and outcomes.
Understanding these rates helps couples make informed decisions. They can weigh the risks and benefits of starting IVF at different ages.
Risks of IVF
Multiple Pregnancies
Multiple pregnancies are a significant risk associated with IVF. This often occurs when more than one embryo is transferred during the procedure. Twin or triplet pregnancies can lead to serious complications for both the mother and the babies.
Higher chances of premature birth arise in multiple pregnancies. Babies born early may face health issues such as respiratory problems or developmental delays. The mother’s health also suffers. Increased risk of gestational diabetes and high blood pressure can occur. Families must weigh these risks against their desire for pregnancy.
Ovarian Hyperstimulation Syndrome (OHSS)
Ovarian hyperstimulation syndrome (OHSS) is another potential risk of IVF. This condition happens when the ovaries react too strongly to fertility medications. Symptoms include abdominal pain, bloating, and nausea. In severe cases, OHSS can lead to serious complications like kidney failure.
The first IVF cycle chance of developing OHSS varies based on individual response to medication. Doctors monitor patients closely to minimize this risk. Adjusting medication doses helps manage symptoms effectively.
Emotional Stress
Emotional stress is a common aspect of undergoing IVF treatment. The journey can be long and filled with uncertainty. Many individuals experience anxiety about the outcome of their first IVF cycle chance. Success is not guaranteed, and repeated attempts may be necessary.
Feelings of disappointment can arise after unsuccessful cycles. Couples often struggle with feelings of inadequacy or frustration. Support from friends, family, or counseling can help navigate these emotions.
Financial Burden
The costs associated with IVF can add another layer of stress. Each cycle typically ranges from $10,000 to $15,000 in the United States alone. Many insurance plans do not cover infertility treatments fully. This financial burden can create tension between partners.
e couples may need multiple cycles to achieve pregnancy, increasing overall expenses. The pressure to succeed quickly adds to emotional strain. Budgeting for treatment and exploring financing options become essential steps for many families.
Tips to Improve IVF Success
Healthy Weight
Maintaining a healthy weight plays a crucial role in IVF success. Studies show that women with a BMI in the normal range have better chances of a successful pregnancy. A balanced diet contributes to overall health. Focus on fruits, vegetables, whole grains, and lean proteins.
Weight management can also affect hormone levels. Hormones influence ovulation and embryo quality. Thus, achieving a healthy weight before starting IVF can improve outcomes.
Balanced Diet
A balanced diet supports reproductive health. Include foods rich in antioxidants, vitamins, and minerals. These nutrients help protect eggs and sperm from damage. Foods high in omega-3 fatty acids are beneficial too. They support hormonal balance and improve blood flow.
Consider incorporating folic acid into your diet. It is essential for fetal development and may enhance fertility. Leafy greens, beans, and fortified cereals are good sources of folic acid.
Avoiding Harmful Substances
Avoiding alcohol, smoking, and excessive caffeine is vital for improving IVF success rates. Alcohol can disrupt hormone levels and impact egg quality. Smoking is linked to reduced fertility in both men and women. It can lead to complications during pregnancy as well.
Caffeine intake should be limited as well. Studies suggest that high caffeine consumption may affect implantation rates. Aim for no more than one or two cups of coffee per day.
Stress Reduction
Stress can negatively impact fertility treatments like IVF. Engaging in stress-reducing activities is important for emotional wellbeing. Techniques such as yoga or meditation can help calm the mind.
Yoga promotes relaxation and improves blood circulation. It also enhances flexibility and strength, which benefits overall health. Meditation aids in reducing anxiety and focusing on positive outcomes.
Finding time for hobbies or activities you enjoy can also lower stress levels. Consider spending time outdoors or with loved ones to foster a supportive environment.
Following Guidelines
Following established guidelines from healthcare professionals is crucial for improving IVF success rates. Consult with your doctor about your treatment plan. They can provide personalized recommendations based on your health history.
Regular check-ups during the IVF process ensure everything is on track. Your doctor may suggest additional tests if needed.
Choosing the Right Fertility Team
Research Success Rates
Successful fertility treatments begin with research. Clinics often publish their success rates online. These rates indicate how many patients achieve live births. Look for clinics that provide transparent data. Check if they report on different fertility treatments, including IVF and ICSI. Patient reviews also offer valuable insights. They can reveal the quality of care and support provided by the clinic.
Experience Matters
Experience plays a crucial role in reproductive technology procedures. A team with specialized training in IVF can make a difference. Many clinics employ board-certified reproductive endocrinologists. Their expertise can enhance treatment outcomes. Ask about the team’s experience with specific infertility problems. Inquire how many cycles they perform each year. This information helps gauge their proficiency in assisted reproductive technologies.
Support Services
Support services are essential when navigating fertility treatments. Clinics should offer counseling to assist patients emotionally. Infertility can be stressful, and having someone to talk to is vital. Financial planning services are equally important. Understanding costs associated with different fertility treatments helps in making informed decisions. An infertility insurance advisor can clarify coverage options as well.
Consider Fertility Preservation
Fertility preservation may be an option for some individuals or couples. This process allows patients to freeze eggs or embryos for future use. It is especially beneficial for those facing health issues or delaying parenthood for personal reasons. Discuss this option with your fertility team if it applies to you.
Evaluate Clinic Guidelines
Fertility guidelines vary between clinics. Each facility may have unique protocols that affect treatment success. Review these guidelines carefully before committing to a clinic. Some clinics may focus on holistic approaches, while others rely heavily on technology. Ensure their approach aligns with your values and preferences.
Understand Treatment Options
Different fertility treatments exist, each with its own set of benefits and challenges. Assisted reproductive technology includes methods like IVF, ICSI, and egg donation. Knowing all available options is crucial for making informed choices about your path forward.
Últimas consideraciones
Navigating IVF can be overwhelming, but understanding the process and success rates empowers you. Factors like age and health play a crucial role in outcomes. By choosing the right fertility team and following tips to boost your chances, you can enhance your journey toward parenthood.
Stay informed and proactive. Knowledge is your best ally in this process. Connect with healthcare professionals, ask questions, and seek support. Your path to success starts with taking the first step. Explore your options and make decisions that align with your goals. You’ve got this!
Frequently Asked Questions
What is IVF?
In vitro fertilization (IVF) is a reproductive technology that helps couples conceive. It involves fertilizing an egg with sperm outside the body and then transferring the embryo to the uterus.
Who is a candidate for IVF?
IVF is suitable for individuals facing infertility due to various reasons, including blocked fallopian tubes, male factor infertility, or unexplained infertility. Consulting a fertility specialist can help determine eligibility.
How do I discuss IVF with my GP?
Start by expressing your concerns about fertility. Ask about potential tests and treatments. Your GP can refer you to a fertility specialist for further evaluation and personalized advice.
What are the main factors affecting IVF success?
Key factors include age, ovarian reserve, sperm quality, lifestyle choices, and the cause of infertility. Each plays a crucial role in determining the likelihood of successful conception.
What are the IVF success rates by age?
Success rates vary by age. Generally, women under 35 have the highest success rates, around 40%. Rates decline significantly after age 40, often below 10%.
What risks are associated with IVF?
Risks include multiple pregnancies, ovarian hyperstimulation syndrome (OHSS), and emotional stress. Discuss potential risks with your healthcare provider before proceeding with treatment.
How can I improve my chances of IVF success?
Maintain a healthy lifestyle, manage stress, avoid smoking and excessive alcohol, and follow your fertility team’s recommendations. Regular check-ups and open communication can also enhance outcomes.
