Posted February 23, 2025 in Fertility Blog & Information
17 minute read

Preimplantation genetic testing (PGT) is a game-changer in reproductive technology. It allows couples to screen embryos for genetic disorders before implantation. This process began in the late 20th century and has evolved rapidly. PGT offers hope for those facing genetic challenges, ensuring healthier pregnancies and reducing the risk of inherited diseases.
With advancements in science, more families can now make informed decisions about their future. PGT not only enhances the chances of successful pregnancies but also empowers parents to choose the healthiest embryos. As awareness grows, so does the importance of understanding this vital procedure. Discover how PGT can transform your journey to parenthood.
Key Takeaways
- Preimplantation genetic testing (PGT) helps identify genetic issues in embryos, improving the chances of a successful IVF outcome.
- Understanding the different biopsy techniques, such as polar body and blastocyst biopsies, is essential for selecting the best approach for your situation.
- Noninvasive PGT (niPGT) is an exciting advancement that can assess the chromosomal makeup of embryos without harming them, making it a safer option.
- Couples considering IVF should discuss PGT with their healthcare provider to understand its benefits and implications for their family planning.
- Staying informed about the latest advances in PGT can help you make better decisions regarding fertility treatments and enhance your chances of success.
- Always prioritize safety and accuracy when choosing a PGT method to ensure the best outcomes for you and your future children.
Understanding Preimplantation Genetic Testing
Definition
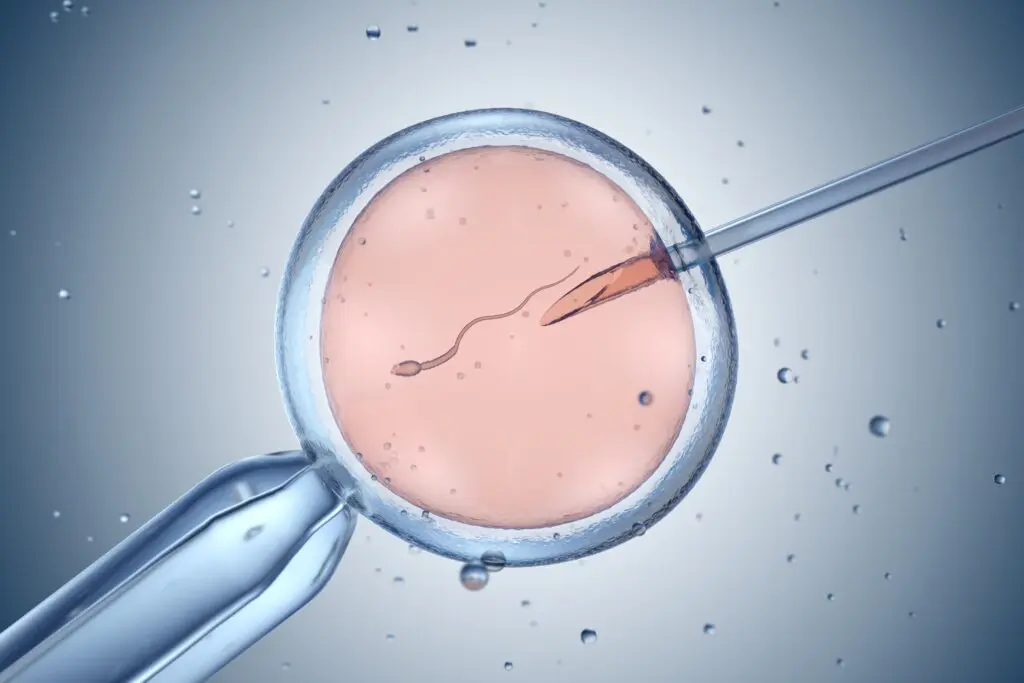
Preimplantation Genetic Testing (PGT) is a technique. It identifies genetic abnormalities in embryos before they are implanted in the uterus. This testing occurs during in vitro fertilization (IVF). By examining the embryos, doctors can determine which ones are genetically healthy.
Types of PGT
PGT has two main types: PGT-A and PGT-M.
PGT-A stands for Preimplantation Genetic Testing for Aneuploidy. It tests embryos for an abnormal number of chromosomes. An abnormality can lead to conditions like Down syndrome or miscarriage. This testing helps select embryos with the correct chromosome number.
PGT-M refers to Preimplantation Genetic Testing for Monogenic Disorders. It focuses on specific genetic disorders passed down in families. Examples include cystic fibrosis and sickle cell disease. Couples with a known risk of these disorders can benefit from this testing. It ensures that only embryos without these genetic conditions are chosen for implantation.
Role in IVF Outcomes
PGT plays a vital role in improving IVF outcomes. Selecting genetically healthy embryos increases the chances of a successful pregnancy. Studies show that using PGT can lead to higher live birth rates. For example, a study published in 2019 found that couples using PGT had about a 70% chance of success compared to 40% without it.
By identifying embryos with genetic issues, PGT reduces the risk of miscarriage. Couples often face emotional stress when dealing with failed pregnancies. PGT offers hope by allowing them to choose healthier embryos.
The process starts with IVF, where eggs are fertilized outside the body. After several days, embryologists assess the embryos’ development. They then perform PGT on the best candidates. Only those that pass the genetic tests proceed to implantation.
Many clinics now offer PGT as part of their IVF services. This option allows parents to make informed choices about their future family. They can avoid passing on serious genetic conditions.
Importance in IVF Success
Benefits for Older Women
PGT-A significantly benefits women of advanced maternal age. As women age, the quality of their eggs often declines. This decline can lead to lower live birth rates and higher miscarriage rates. PGT-A helps identify embryos with the best chance of success. Studies show that it improves live birth rates by selecting genetically normal embryos. This is crucial for older women who may face more challenges during IVF.
Women using PGT-A often see a reduction in miscarriage rates. Traditional IVF methods do not provide this level of insight into embryo viability. By choosing embryos that are less likely to result in miscarriage, women increase their chances of having a healthy pregnancy.
Elective Single Embryo Transfer
One major advantage of PGT-A is the option for elective single embryo transfer (eSET). This method involves transferring only one embryo at a time. eSET has become popular due to its effectiveness. It increases live birth rates per cycle while minimizing risks associated with multiple births.
Transferring multiple embryos can lead to complications for both mother and babies. With eSET, women can achieve similar success rates as traditional two-embryo transfers, but with fewer risks. This is especially important for older women who may already face higher risks during pregnancy.
Shortening Time to Pregnancy
PGT also plays a vital role in shortening the time to pregnancy. Identifying viable embryos early allows couples to focus on those with the highest potential for implantation. This efficiency can save time and emotional stress during the IVF process.
Couples often go through multiple cycles before achieving a successful pregnancy. PGT-A reduces this uncertainty by pinpointing which embryos are genetically normal from the start. By doing so, it streamlines the process and provides hope for quicker results.
The use of preimplantation genetic testing can transform the IVF experience for many couples. It offers clearer insights into embryo health, leading to informed decisions about transfers.
Overview of Biopsy Techniques
Polar Body Biopsy
This technique involves removing the polar body from the egg. A polar body is a small cell that forms during oocyte maturation. It contains genetic material from the mother.
Polar body biopsy occurs before fertilization. It allows for testing of maternal genes without touching the embryo itself. This method helps identify genetic abnormalities in the mother’s contribution. It provides insight into conditions like mitochondrial diseases, which can affect pregnancy outcomes.
Cleavage-Stage Embryo Biopsy
Cleavage-stage embryo biopsy takes place on day 3 after fertilization. At this stage, the embryo typically has six to eight cells. Technicians carefully remove one or two cells from the embryo for analysis.
The purpose of this technique is to obtain genetic material for testing. Removing cells at this point gives insight into potential genetic disorders. Scientists analyze these cells to determine if there are any chromosomal abnormalities. This method helps in selecting viable embryos for transfer, increasing IVF success rates.
Blastocyst Biopsy
Blastocyst biopsy is performed on day 5 or 6 of embryo development. By this stage, the embryo has developed into a structure with over 100 cells. The blastocyst consists of an inner cell mass and an outer layer called the trophectoderm.
This technique focuses on extracting cells from the trophectoderm. These cells provide a comprehensive view of the embryo’s genetic health. Testing at this stage allows for more accurate results compared to earlier techniques. It also enables selection of embryos with the highest potential for implantation.
Polar Body Biopsy Explained
Purpose
Polar body biopsy is a technique used to analyze female chromosomal disorders. This method examines the polar bodies, which are small cells produced during egg development. Each egg releases two polar bodies, and these contain genetic material from the mother.
Chromosomal Analysis
This technique provides information on the chromosomal content of the egg. By analyzing the polar bodies, doctors can determine if the egg has any chromosomal abnormalities. This is crucial for women who may be at risk of passing on genetic disorders. The analysis helps in making informed decisions about fertility treatments.
Limitations
Polar body biopsy does not give information about the subsequent embryo. While it can indicate whether an egg is healthy, it cannot predict how the embryo will develop after fertilization. The embryo’s genetic makeup may differ from that of the polar bodies. This limitation means that while the technique is useful, it is not foolproof.
Process Overview
The process begins with egg retrieval during an in vitro fertilization (IVF) cycle. Once retrieved, specialists identify and isolate the polar bodies from each egg. They then analyze these cells using various techniques, such as fluorescent in situ hybridization (FISH). FISH allows for the visualization of specific chromosomes.
Clinical Applications
Doctors often recommend this method for women over 35 or those with a history of genetic disorders. It helps in identifying viable eggs before fertilization. Couples can use this information to select healthier embryos for implantation.
Advantages
- Informed Decisions: Couples can make better choices regarding IVF procedures.
- Reduced Risk: It lowers the chances of genetic disorders in future pregnancies.
- Cost-Effective: By selecting healthier eggs, couples may reduce the need for multiple IVF cycles.
Challenges
- Limited Information: It does not provide data on embryo viability.
- Technical Skill Required: The procedure requires highly trained professionals.
- Emotional Impact: Couples may face stress over testing results.
Cleavage-Stage Embryo Biopsy Details
Cell Removal
Cleavage-stage biopsy involves the removal of one or two cells from a day 3 embryo. This stage occurs around 72 hours after fertilization. At this point, the embryo typically has six to eight cells. Removing a cell can provide critical genetic information about the embryo.
This technique allows for early genetic testing. It helps identify potential genetic disorders before implantation. However, it is important to note that this method may impact embryo development. Removing cells can stress the embryo, potentially affecting its ability to implant successfully.
Genetic Testing Benefits
Early genetic testing through cleavage-stage biopsy offers several advantages. Parents can make informed decisions about their embryos. They can select embryos with the best chances for healthy development. This leads to higher success rates in assisted reproductive technologies.
Genetic testing also helps prevent the transmission of inherited diseases. For instance, conditions like cystic fibrosis or Tay-Sachs disease can be detected early. By identifying these issues, parents can avoid passing them on to their children.
Mosaicism Concerns
Mosaicism presents a significant concern in cleavage-stage biopsies. This condition occurs when different cells in an embryo have different genetic compositions. Not all cells may carry the same mutations or abnormalities.
For example, one cell may show signs of a genetic disorder while another does not. This can lead to confusion regarding the embryo’s overall health. Some studies suggest that mosaic embryos can still develop normally. However, the outcomes remain uncertain.
Implications for Embryo Development
The implications of using cleavage-stage biopsy are complex. While it provides valuable information, it also raises questions about embryo viability. The removal of cells might disrupt normal development processes.
Research indicates that embryos subjected to biopsy might have lower implantation rates compared to those that are not biopsied. This could lead to fewer successful pregnancies overall.
Blastocyst Biopsy Insights
Cell Removal
Blastocyst biopsy involves taking cells from the trophectoderm layer of a day 5 embryo. This layer surrounds the inner cell mass, which will eventually form the fetus. By removing these cells, doctors can analyze the genetic material without harming the developing embryo.
This technique is more advanced than earlier methods. It allows for better genetic analysis of embryos before implantation. The procedure typically occurs on day 5 of development when the embryo reaches the blastocyst stage. At this point, the embryo has developed enough to provide a reliable sample.
Comprehensive Analysis
The comprehensive genetic analysis provided by blastocyst biopsy is a key advantage. Testing at this stage gives more information about the embryo’s health and viability. This method can identify chromosomal abnormalities and genetic disorders that could affect future pregnancies.
Less risk to the embryo is another significant benefit. While previous techniques might have affected embryo quality, blastocyst biopsy minimizes this risk. This approach leads to higher success rates in assisted reproductive technologies.
Safety and Accuracy
Safety and accuracy are critical factors in preimplantation genetic testing (PGT). Blastocyst biopsy is now the most commonly used method for PGT due to its reliability. Studies show that it has a lower chance of damaging embryos compared to cleavage-stage biopsies.
Doctors prefer this technique because it provides clear results. The accuracy helps in making informed decisions about which embryos to implant. Higher accuracy means fewer chances of miscarriage or genetic disorders in live births.
Procedure Steps
- Embryo culture: Embryos develop for five days in a controlled environment.
- Biopsy: A small number of trophectoderm cells are removed.
- Genetic testing: The cells undergo analysis for chromosomal or genetic issues.
- Implantation: Only healthy embryos are selected for transfer into the uterus.
This process highlights how advancements in technology improve reproductive options for couples facing genetic challenges.
Assessing Chromosomal Makeup
Importance of Assessment
Assessing chromosomal makeup is crucial in the context of preimplantation genetic testing. This evaluation helps identify aneuploid embryos. Aneuploidy refers to an abnormal number of chromosomes. It can lead to complications such as failed implantation or miscarriage.
Around 50% of embryos created through in vitro fertilization (IVF) show chromosomal abnormalities. These abnormalities can prevent a successful pregnancy. By identifying these issues early, patients can avoid unnecessary emotional and financial stress associated with failed pregnancies.
Role of PGT-A
Preimplantation Genetic Testing for Aneuploidy (PGT-A) plays a key role in detecting chromosomal abnormalities. This test analyzes the chromosomes of embryos before implantation. PGT-A uses advanced techniques to evaluate each embryo’s genetic composition.
The process begins with a biopsy of the blastocyst, which was discussed previously. After obtaining cells, genetic analysis occurs. This analysis reveals whether an embryo has the correct number of chromosomes. If an embryo is identified as euploid, it means it has a normal chromosome number. This significantly increases the chances of successful implantation and healthy pregnancy.
Embryos that are aneuploid often do not implant or may lead to miscarriage if they do implant. Studies show that using PGT-A can reduce the risk of miscarriage by selecting only healthy embryos for transfer.
Genetic Counselors’ Role
Genetic counselors play a vital role in interpreting PGT results. They help patients understand their options based on genetic findings. Patients often feel overwhelmed after receiving PGT results. Counselors provide clarity and support during this time.
They explain what the results mean for future pregnancies. If an embryo is found to be aneuploid, counselors discuss potential next steps. They guide patients on whether to use other viable embryos or consider different reproductive options.
Genetic counselors also address emotional aspects related to testing outcomes. Many patients experience anxiety about their fertility journey. Counselors offer resources and coping strategies tailored to individual needs.
Advances in Noninvasive PGT
niPGT Overview
Noninvasive preimplantation genetic testing (niPGT) is a method that studies cell-free DNA found in the culture medium. This technique allows for the analysis of genetic material without directly sampling the embryo. Researchers collect this DNA from the fluid surrounding embryos during in vitro fertilization (IVF). This process minimizes any direct intervention with the embryos.
Reduced Risks
Using niPGT reduces the need for embryo biopsy. Traditional methods involve extracting cells from the embryo, which can pose risks. These risks include potential damage to the embryo and lower implantation rates. By avoiding invasive procedures, niPGT aims to protect the embryo’s integrity. This advancement represents a significant shift in how genetic testing is performed during IVF.
Ongoing Research
Ongoing research continues to explore the effectiveness of niPGT. Scientists are studying how well it predicts chromosomal abnormalities compared to traditional methods. Early studies suggest that niPGT may provide reliable results while minimizing risks associated with invasive techniques.
A 2020 study published in “Human Reproduction” showed promising outcomes with niPGT. The results indicated that this method could effectively identify embryos with genetic issues without harming them. As more data becomes available, researchers hope to refine these techniques further.
Improving IVF Outcomes
The promise of niPGT lies in its potential to improve IVF outcomes. With less risk involved, more couples may consider genetic testing as part of their fertility treatment. Successful identification of healthy embryos can lead to higher implantation rates and fewer miscarriages. This could ultimately result in more successful pregnancies.
Another advantage is the possibility of earlier detection of genetic disorders. Couples can make informed decisions about their options before implantation. This proactive approach helps reduce emotional stress during the IVF process.
Future Prospects
Looking ahead, researchers aim to enhance niPGT technologies. Improvements may include better algorithms for analyzing DNA and refining laboratory techniques. The goal is to increase accuracy and reliability while maintaining noninvasiveness.
As knowledge expands, healthcare providers may adopt niPGT more widely. This could transform standard practices in reproductive medicine. The future of noninvasive genetic testing appears bright and full of potential.
Safety and Accuracy in niPGT
Importance of Validation
Ensuring the accuracy of noninvasive preimplantation genetic testing (niPGT) results is crucial. Rigorous validation studies play a key role in this process. These studies assess how well niPGT can detect genetic conditions before embryo implantation. They also compare niPGT results with traditional invasive methods, such as amniocentesis.
Validation studies help identify any potential errors in niPGT. By confirming its accuracy, medical professionals can trust the results more. This trust is essential for patients who rely on these tests to make informed decisions about their pregnancies.
Benefits for Patients
niPGT offers several benefits that enhance patient safety. It reduces the need for invasive procedures that carry risks. Traditional methods like chorionic villus sampling (CVS) can lead to complications, including miscarriage. With niPGT, patients avoid these risks while still receiving valuable genetic information.
NiPGT can provide quicker results than invasive tests. Faster results mean patients can make timely decisions regarding their treatment options. This speed can be critical for those facing difficult choices about their pregnancy.
Technological Advancements
Continued advancements in technology are necessary to improve the reliability of niPGT. As techniques evolve, so does the ability to detect a broader range of genetic conditions. New technologies can enhance the sensitivity and specificity of tests. This means fewer false positives and negatives.
For example, improvements in sequencing technology have already shown promise. Enhanced sequencing methods allow for more accurate analysis of cell-free fetal DNA from maternal blood samples. These advancements lead to better outcomes for patients and their families.
Research into artificial intelligence (AI) also holds potential. AI can analyze large datasets quickly and accurately. This capability may help refine testing processes and improve result interpretations.
Future Considerations
The future of niPGT looks promising but requires ongoing research and development. Regulatory bodies must continue to evaluate safety standards and effectiveness. This oversight ensures that new technologies meet high-quality benchmarks before they reach patients.
Education for healthcare providers is equally important. Professionals must stay updated on the latest advancements in niPGT to guide patients effectively. Clear communication about what niPGT can and cannot do will empower patients in their decision-making process.
Closing Thoughts
Preimplantation genetic testing (PGT) plays a crucial role in enhancing your IVF journey. By understanding the various biopsy techniques and advances in noninvasive methods, you can make informed decisions about your reproductive health. Safety and accuracy are paramount, ensuring that you choose the best options for your needs.
Embrace the potential of PGT to improve your chances of a successful pregnancy. Stay informed, ask questions, and consult with experts to navigate this complex landscape. Your path to parenthood can be clearer with the right knowledge and support. Take charge of your fertility journey today!
Frequently Asked Questions
What is Preimplantation Genetic Testing (PGT)?
Preimplantation Genetic Testing (PGT) is a procedure used in IVF to screen embryos for genetic abnormalities before implantation. It helps identify healthy embryos, increasing the chances of a successful pregnancy.
Why is PGT important for IVF success?
PGT enhances IVF success by selecting genetically viable embryos. This reduces the risk of miscarriage and increases the likelihood of a healthy pregnancy, ultimately saving time and resources for prospective parents.
What are the different biopsy techniques used in PGT?
The main biopsy techniques include Polar Body Biopsy, Cleavage-Stage Embryo Biopsy, and Blastocyst Biopsy. Each method targets specific stages of embryo development to assess genetic health effectively.
How does Polar Body Biopsy work?
Polar Body Biopsy involves extracting polar bodies from an egg prior to fertilization. This technique provides information about the maternal genetic contribution without harming the embryo itself.
What occurs during a Cleavage-Stage Embryo Biopsy?
During a Cleavage-Stage Embryo Biopsy, one or two cells are removed from an embryo at the 6-8 cell stage. This allows for genetic testing while preserving the embryo’s viability for implantation.
What insights can be gained from Blastocyst Biopsy?
Blastocyst Biopsy occurs at a later developmental stage when the embryo has formed a blastocyst. This technique offers more comprehensive genetic information, improving selection accuracy for implantation.
How does noninvasive PGT (niPGT) differ from traditional methods?
Noninvasive PGT (niPGT) analyzes genetic material from the culture media surrounding embryos instead of directly sampling them. This method reduces risks associated with invasive procedures while maintaining high accuracy in genetic assessment.
