Posted October 16, 2024 in Fertility Blog & Information
18 minute read
Understanding the fertility treatment timeline, including the fertilization cycle and the first ivf cycle, is crucial for anyone navigating this journey. Over the years, advancements in reproductive medicine, including advanced fertility treatments, fertilization beginning, embryo culturing preimplantation genetic testing, and uterine preparation, have made it possible for many to achieve their dreams of parenthood. The process can vary significantly day by day based on individual circumstances, medical history, and chosen treatments.
From initial consultations to various procedures like IVF or IUI, each step plays a vital role in the overall timeline. Knowing what to expect at each phase can ease anxiety and help you make informed decisions. This post will break down the fertility treatment timeline, providing insights and tips to support your path toward conception.
Key Takeaways
- Understand the IVF process thoroughly to know what to expect at each stage, which can help reduce anxiety and improve your experience.
- Familiarize yourself with the various stages of the IVF cycle, as this knowledge can assist you in planning and managing your time effectively.
- Recognize the factors that can influence the duration of IVF, such as age and health conditions, to set realistic expectations for your treatment timeline.
- Prepare for IVF by undergoing key fertility tests and following pre-IVF health measures, which can enhance your chances of success.
- Implement practical tips for IVF preparation, like maintaining a healthy lifestyle and staying organized, to create a supportive environment for your treatment.
- Monitor your pregnancy closely post-IVF, as early detection of any issues can lead to better outcomes and peace of mind.
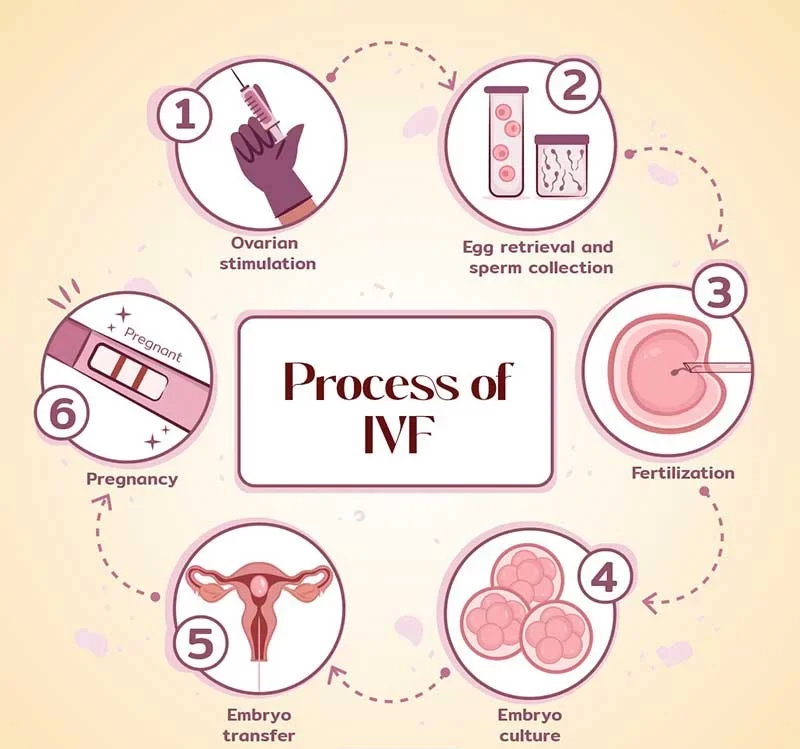
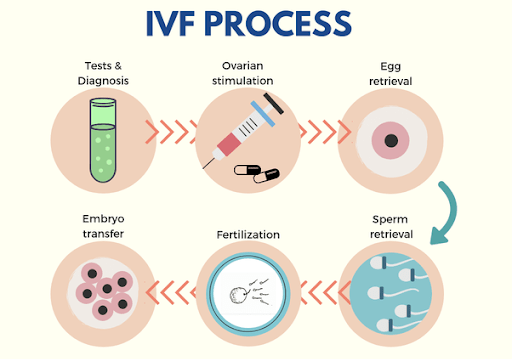
Understanding the IVF Process
IVF Basics
IVF stands for In Vitro Fertilization. This is a fertility treatment that helps women conceive. It involves combining eggs and sperm outside the body. The process takes place in a laboratory. Once fertilized, the embryos are placed back into the woman’s uterus.
Primary Steps
- Ovarian Stimulation: Doctors give women hormone injections. These hormones help produce multiple eggs instead of one.
- Egg Retrieval: After the eggs mature, doctors perform a minor surgical procedure to collect them. This is done using a thin needle guided by ultrasound.
- Insemination Procedure: The collected eggs are mixed with sperm in a lab dish. This allows fertilization to occur.
- Embryo Culture: Fertilized eggs develop into embryos over several days. Doctors monitor their growth closely.
- Preimplantation Genetic Screening Process: Some couples choose to test embryos for genetic conditions before implantation. This step helps ensure healthy pregnancies.
- Embryo Transfer: One or more healthy embryos are selected and transferred into the uterus. This is done through a thin tube called a catheter.
- Pregnancy Test: About two weeks later, women take a blood test to check for pregnancy.
Purpose and Goals
The main goal of IVF is to help couples achieve pregnancy when other methods have failed. Many factors can lead to infertility, including age, health issues, or unexplained reasons. IVF provides hope for families wanting children.
Women undergoing IVF often face emotional challenges. The process can be stressful and requires patience. Support from partners and medical teams plays an important role in this journey.
Success rates vary based on age and health conditions. Younger women generally have higher success rates compared to older women. Each cycle can also be expensive, which adds financial stress to couples.
Ultimately, IVF aims to create life where it might not happen naturally. Many families have welcomed healthy babies through this method. For those struggling with fertility, IVF offers a chance at parenthood that may otherwise seem out of reach.
Stages of the IVF Cycle
Stimulation Phase
The stimulation phase is the first step in the IVF process. It usually lasts about 10 to 14 days. Doctors prescribe hormone medications to encourage the ovaries to produce multiple eggs. These medications often include follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Regular monitoring is crucial during this phase. Patients undergo blood tests and ultrasounds to track hormone levels and follicle growth. The goal is to ensure that follicles develop properly. When follicles reach an appropriate size, it signals that they are ready for egg retrieval.
Egg Retrieval Process
Egg retrieval occurs once the follicles are mature. This typically happens about 34-36 hours after administering a trigger shot of human chorionic gonadotropin (hCG). The trigger shot helps finalize the maturation of the eggs.
During the procedure, a thin needle is inserted through the vaginal wall into each follicle. Ultrasound guides this process. A sedative is given to minimize discomfort. The doctor extracts the eggs from the follicles. This procedure usually lasts around 20-30 minutes. After retrieval, doctors assess how many viable eggs were collected.
Fertilization Stage
The next step involves fertilization. This typically occurs within a few hours after egg retrieval. Eggs are combined with sperm in a lab setting. There are two main methods: conventional insemination and intracytoplasmic sperm injection (ICSI). In conventional insemination, sperm and eggs are placed together in a dish and allowed to fertilize naturally.
In cases where there are concerns about sperm quality, ICSI may be used. Here, a single sperm is injected directly into an egg. This method increases the chances of fertilization.
After fertilization, embryos begin developing. This stage lasts about five to six days. Embryos go through several stages, including the cleavage stage and blastocyst stage. During the cleavage stage, cells divide rapidly. By day five or six, some embryos reach the blastocyst stage, which indicates they have developed further.
Doctors monitor embryo development closely. Only the strongest embryos are selected for transfer into the uterus. This selection process is crucial for increasing chances of pregnancy.
Factors Influencing IVF Duration
Medication Response
The response to medications varies widely among individuals. Some may react quickly, while others take longer. This variability can affect the overall timeline of in vitro fertilization (IVF).
For instance, ovarian stimulation medications are crucial. They help stimulate the ovaries to produce eggs. The time it takes for these medications to work can differ based on individual biology. Some women might respond within a few days, while others may require several weeks.
Monitoring is essential during this phase. Doctors often perform blood tests and ultrasounds to track progress. These evaluations help determine if adjustments are needed in medication dosages. A personalized approach ensures that each patient receives the most effective treatment.
Age Factor
Age plays a significant role in IVF duration. Younger women tend to have more responsive ovaries. They often produce more eggs in a shorter timeframe compared to older women.
Research shows that women under 35 generally have better outcomes with IVF. Their bodies typically respond faster to treatments. In contrast, women over 40 may face longer timelines due to decreased egg quality and quantity.
Health conditions also impact how quickly someone can undergo IVF. Conditions like polycystic ovary syndrome (PCOS) or endometriosis can complicate matters. These factors can lead to extended durations for medication adjustments and monitoring.
Health Conditions
Individual health conditions influence IVF duration as well. Each patient’s medical history is unique and must be considered during treatment planning.
e conditions may require additional testing before starting IVF. For example, hormonal imbalances need correction prior to ovarian stimulation. This could add weeks to the overall timeline.
Doctors often create tailored treatment plans based on these health factors. A personalized plan addresses specific needs and aims for the best outcomes.
Personalized Treatment Plans
Personalized treatment plans are crucial for optimizing IVF success rates. Each patient’s journey through IVF is different. Customizing treatment helps manage expectations and timelines effectively.
A comprehensive evaluation at the start helps identify individual needs. This assessment includes hormone levels, age, and any existing health issues.
By tailoring the approach, fertility specialists can address unique challenges faced by each patient. This strategy not only enhances effectiveness but also minimizes unnecessary delays.
In summary, several factors influence the duration of IVF treatments. Variability in medication response times, age-related considerations, and individual health conditions all play a role. Personalized treatment plans are vital for navigating this complex process efficiently.
Preparing for IVF
Medical Evaluation
A thorough medical evaluation is essential before starting in vitro fertilization (IVF). This process often begins with a consultation with a fertility specialist. The specialist will assess medical history and conduct necessary tests. Blood tests, ultrasounds, and physical exams help identify potential issues.
Understanding any underlying health conditions is crucial. Conditions like polycystic ovary syndrome (PCOS) or endometriosis can affect treatment plans. A fertility nurse may guide you through this evaluation. They provide support and answer questions about the process.
Lifestyle Changes
Making lifestyle changes can improve IVF outcomes. Diet plays a significant role in fertility health. Eating a balanced diet rich in fruits, vegetables, and whole grains is beneficial. Maintaining a healthy weight also supports reproductive health.
Regular exercise helps too. Aim for moderate activity like walking or swimming. Reducing alcohol intake and quitting smoking are vital steps as well. These changes can enhance ovarian preparation and overall health during treatment.
Stress management is another important aspect. Practices such as yoga or meditation can help reduce anxiety levels. Lower stress may lead to better responses to fertility medications.
Understanding the Timeline
Understanding the IVF timeline is critical for commitment. The entire process can span several weeks to months. It includes multiple steps such as ovarian stimulation, egg retrieval, and embryo transfer.
Ovarian preparation typically starts with fertility medications to stimulate egg production. This phase lasts about 10-14 days. Monitoring occurs frequently through blood tests and ultrasounds during this time.
Once eggs are retrieved, they undergo insemination in an IVF lab. Fertilized eggs develop into embryos over several days. Some clinics offer preimplantation genetic testing to screen embryos for genetic disorders.
After culturing embryos, the next step involves transferring them into the uterus. A fresh embryo transfer usually occurs within five days post-retrieval. However, some choose to freeze embryos for future use.
Planning for these steps requires understanding both time and emotional investment. Couples facing infertility challenges should prepare for possible ups and downs throughout the journey.
Commitment Required
Commitment is essential in navigating difficult infertility cases. Each stage of IVF demands attention and dedication from both partners. Staying informed about procedures helps ease anxiety.
Working closely with expert fertility nurses provides additional support throughout the process. They offer guidance on medication schedules and what to expect at each stage.
Being aware of IVF costs is also vital when preparing financially for treatment. Costs can vary widely based on location and specific services needed.
Key Fertility Tests
Initial Testing
Initial fertility testing is crucial for couples trying to conceive. This stage often involves a standard fertility evaluation. Doctors typically recommend this after a year of unsuccessful attempts for women under 35 and after six months for those over 35.
Common tests include blood tests, ultrasounds, and semen analysis. Blood tests measure hormone levels. These hormones play significant roles in ovulation and reproductive health.
Ultrasounds help visualize the ovaries and uterus. They can identify issues like cysts or fibroids that may affect fertility. Semen analysis evaluates sperm count, motility, and morphology. This test assesses male fertility factors.
Blood Tests
Blood tests are essential in assessing reproductive health. They check hormone levels like FSH, LH, estradiol, and progesterone. Each hormone has a specific function in the menstrual cycle.
FSH (Follicle-Stimulating Hormone) helps determine ovarian reserve. High levels may indicate diminished egg supply. LH (Luteinizing Hormone) triggers ovulation. Estradiol indicates how well the ovaries function.
Progesterone is vital for maintaining pregnancy. Low levels can signify problems with ovulation or early pregnancy loss. Doctors use these results to understand a patient’s specific fertility needs.
Ultrasounds
Ultrasounds provide a clear view of reproductive organs. They help assess the health of the uterus and ovaries. Transvaginal ultrasounds are common for fertility evaluations.
These tests can detect structural issues such as polyps or endometriosis. Finding these conditions early can lead to more effective treatment plans. Doctors can tailor IVF strategies based on ultrasound findings.
Tailoring IVF Plans
Fertility testing plays a critical role in forming individualized IVF treatment plans. Each couple’s situation is unique, requiring specific approaches.
Successful IVF depends on understanding both partners’ reproductive health. Tests inform doctors about hormonal balances and structural issues that need addressing.
For example, if blood tests reveal low progesterone, doctors may prescribe supplements during IVF cycles. If ultrasounds show fibroids, they might recommend surgical removal before starting IVF.
Pre-IVF Health Measures
Healthy Diet
Maintaining a healthy diet is crucial before starting fertility treatments. A balanced diet supports the body during this time. Foods rich in vitamins and minerals can improve overall health. Fruits, vegetables, whole grains, and lean proteins are essential.
Specific nutrients play vital roles. For instance, folic acid is important for women trying to conceive. This nutrient helps prevent birth defects. Omega-3 fatty acids can also benefit reproductive health. They are found in fish, flaxseeds, and walnuts.
Regular meals help maintain stable blood sugar levels. This stability can reduce cravings and promote better food choices. Proper hydration is equally important. Drinking enough water aids digestion and nutrient absorption.
Regular Exercise
Engaging in regular exercise can enhance fertility outcomes. Physical activity helps maintain a healthy weight. Being overweight or underweight can impact fertility negatively.
Aim for at least 150 minutes of moderate exercise each week. Activities like walking, cycling, or swimming are beneficial. Exercise also improves mood and reduces stress levels.
Strength training is another good option. It builds muscle mass and boosts metabolism. However, avoid excessive exercise as it may have the opposite effect on fertility.
Stress Management
Managing stress is essential for those considering IVF treatments. High stress levels can disrupt hormonal balance. This disruption may affect ovulation and overall reproductive health.
Techniques such as meditation and yoga can be effective. These practices promote relaxation and mental clarity. Mindfulness exercises help individuals focus on the present moment.
Counseling or support groups can provide additional help. Speaking with others who share similar experiences offers emotional support. Sharing feelings can relieve anxiety related to treatment.
Avoid Harmful Substances
Avoiding harmful substances is critical when preparing for IVF procedures. Alcohol consumption can negatively affect fertility for both men and women. Studies show that excessive drinking lowers sperm count in men and affects ovulation in women.
Tobacco use has similar effects. Smoking harms egg quality and reduces fertility rates. Quitting smoking improves chances of conception significantly.
Caffeine intake should also be monitored. Some studies suggest high caffeine consumption may lead to fertility issues. Limiting caffeine to about 200 mg per day is advisable.
Individual Circumstances
Every person’s journey through fertility treatment varies based on individual circumstances. Factors like age, medical history, and lifestyle all play roles in treatment effectiveness.
Costs associated with fertility treatments can vary widely too. Understanding these costs helps individuals plan better financially. It’s essential to consult healthcare providers about specific recommendations tailored to personal needs.
Practical Tips for IVF Preparation
Organizing Medications
IVF involves a strict medication schedule. Start by creating a detailed calendar. Mark the dates for injections and medications. Use reminders on your phone or a planner to stay on track.
Keep all medications in one place. A designated drawer or box can help prevent confusion. Always check if you have enough supplies before each appointment. This ensures you won’t run out unexpectedly.
Managing Appointments
Schedule your appointments well in advance. IVF treatments often require frequent visits to the clinic. Make a list of all necessary tests and procedures.
Consider using a shared calendar with your partner. This allows both of you to keep track of important dates. It also helps in planning time off work or arranging transportation.
Emotional Well-Being
Emotional support is crucial during IVF. Talk openly with your partner about feelings and concerns. Sharing thoughts can reduce stress.
Seek support from friends or family. Joining an IVF support group can provide comfort. Others understand what you’re going through and can share their experiences.
Practice relaxation techniques such as yoga or meditation. These methods can help manage anxiety and improve mental health.
Financial Planning
IVF can be expensive, so financial planning is important. Research costs associated with treatment early on. Create a budget that includes medication, procedures, and consultations.
Check if your insurance covers any part of the treatment. Some plans may offer partial reimbursement for fertility treatments. Knowing this information can help ease financial pressure.
Consider setting up a savings account specifically for IVF expenses. This strategy allows you to save gradually without feeling overwhelmed by costs.
Timeline Awareness
Understanding the history of IVF can aid in preparation. The first successful IVF birth occurred in 1978, marking a significant milestone in reproductive medicine. Since then, techniques have improved significantly.
Familiarize yourself with the typical timeline of an IVF cycle. It usually lasts about four to six weeks from stimulation to embryo transfer. Knowing what to expect helps reduce anxiety and keeps you focused.
Monitoring Pregnancy Post-IVF
Importance of Monitoring
Monitoring during early pregnancy is crucial. Blood tests help confirm pregnancy. They measure hormone levels, particularly human chorionic gonadotropin (hCG). This hormone is key in supporting the development of the embryo.
Results from blood tests provide valuable information. A rising hCG level indicates a healthy pregnancy. Doctors typically perform these tests about 10 days after embryo transfer. Early detection can help identify potential issues.
Patients often feel anxious during this time. Knowing that medical professionals are monitoring their progress can provide peace of mind. It reassures individuals that they are not alone in this journey.
Role of Ultrasounds
Ultrasounds play a vital role in tracking embryo development. These imaging tests allow doctors to visualize the growing fetus. The first ultrasound usually occurs around six weeks into the pregnancy.
During this ultrasound, doctors check for a heartbeat. This is an important milestone in confirming a viable pregnancy. The presence of a heartbeat often brings relief to expecting parents.
Further ultrasounds follow as the pregnancy progresses. They help monitor growth and development at various stages. Each ultrasound provides critical information about the baby’s health and well-being.
Ongoing Medical Support
Ongoing medical support is essential throughout the pregnancy. Regular check-ups help track both maternal and fetal health. These visits typically begin every four weeks and become more frequent as the due date approaches.
Healthcare providers assess various factors during these visits. They monitor weight gain, blood pressure, and fetal heart rate. This ongoing care ensures that any complications are addressed promptly.
Pregnancy after IVF can present unique challenges. Individuals may face emotional ups and downs during this time. Having a supportive healthcare team can make a significant difference.
Doctors encourage open communication with patients. Discussing concerns or questions helps build trust and ensures comprehensive care. Patients should feel empowered to voice their needs and preferences.
In summary, monitoring during early pregnancy post-IVF is crucial for success. Blood tests confirm pregnancy and track hormonal changes. Ultrasounds provide visual confirmation of embryo development and health milestones.
Regular check-ups offer ongoing support for both mother and baby. This comprehensive approach helps ensure a positive outcome for all involved.
Pensamientos Finales
Navigating the fertility treatment timeline can feel overwhelming. Understanding each stage of the IVF process helps you prepare and set realistic expectations. By knowing what to expect, you can alleviate some of your stress and focus on the journey ahead.
Stay proactive in your preparations and keep open communication with your healthcare team. They are there to guide you through every step. Remember, knowledge is power. Equip yourself with information and take charge of your fertility journey. If you’re ready to take the next steps, consult a specialist today and explore your options. Your path to parenthood starts with informed choices.
Frequently Asked Questions
What is the typical timeline for IVF treatment?
The typical IVF treatment timeline spans about 4 to 6 weeks, including ovarian stimulation, egg retrieval, fertilization, and embryo transfer. However, individual circumstances can extend this duration.
How long does each stage of the IVF process take?
Each stage varies: ovarian stimulation usually takes 10-14 days, egg retrieval occurs shortly after, and embryo transfer happens a few days later. The total timeline can vary based on individual response.
What factors can affect the duration of IVF?
Factors include age, hormonal response, medical history, and clinic protocols. Each patient’s unique situation can lead to variations in the overall timeline.
What health measures should I take before starting IVF?
Before IVF, maintain a healthy diet, exercise regularly, manage stress, and avoid smoking or excessive alcohol. These steps improve your chances of success.
What key fertility tests are necessary before IVF?
Key fertility tests include hormone level assessments, ultrasound examinations, and semen analysis. These tests help identify any underlying issues that may affect treatment.
How can I prepare practically for IVF?
Practical preparation includes organizing your schedule for appointments, understanding medication protocols, and setting up a support system. Being prepared can ease anxiety during the process.
How do I monitor pregnancy after IVF?
Post-IVF pregnancy monitoring typically involves blood tests to check hormone levels and ultrasounds to confirm fetal development. Regular follow-ups with your doctor are crucial for a healthy pregnancy.
