Posted September 10, 2024 in Fertility Blog & Information
16 minute read
The microbiome and fertility connection is a game-changer in reproductive health, particularly for infectious infertility women and infertile women, highlighting the importance of endometrial interaction in cases of primary infertility. Recent research shows that the gut bacteria, along with the tubal microbiome and vagina, can influence hormonal balance and ovulation in men and their health status. This means your microbiome, including that of the vagina, might play a crucial role in your ability to conceive for men.
Understanding this link opens new doors for couples, including men, struggling with fertility issues related to the vagina. By optimizing gut health, you could enhance your chances of pregnancy in men and women, including the vagina. Simple lifestyle changes can make a big impact on your microbiome, including the vagina, leading to better reproductive outcomes for men. Dive into this fascinating topic and discover how nurturing your vagina and microbiome can boost your fertility journey for men.
Key Takeaways
- Understanding the connection between microbiomes in the vagina and fertility in men can help you make informed choices about your reproductive health.
- The genital tract microbiome, including the vagina, plays a crucial role in maintaining a healthy reproductive system for men; consider consulting with a healthcare provider for personalized advice.
- A balanced gut microbiome influences hormone levels in both men and women, so focus on a diet rich in fiber and probiotics to support gut health, including the vagina.
- Immune function is essential for reproductive health in men; managing stress and getting adequate sleep can enhance immune responses.
- Addressing microbiome disorders, such as dysbiosis, may improve fertility outcomes; seek professional guidance if you suspect an imbalance.
- Nutrition and lifestyle changes, like reducing processed foods and incorporating regular exercise, are vital for optimizing microbiome health and boosting fertility.
Understanding Microbiomes and Fertility
Microbiome Definition
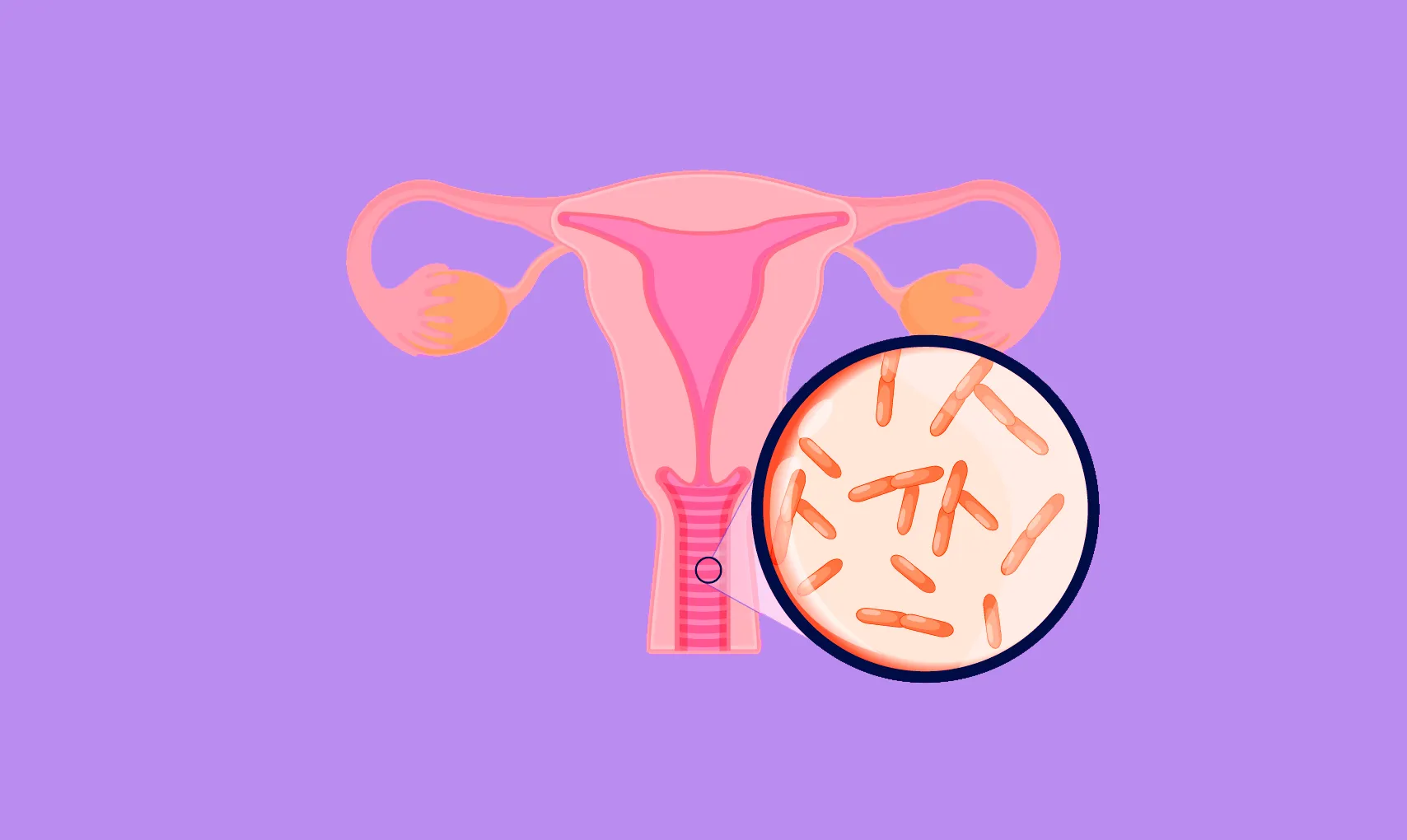
The human microbiome consists of trillions of microbes. These include bacteria, viruses, fungi, and other microorganisms. They live in various parts of the body, including the gut, skin, and genital tract. The microbiome plays a vital role in overall health. It helps with digestion, supports the immune system, and protects against harmful pathogens.
Genital Tract Impact
The endometrial microbiome refers to the microbial community within the uterine cavity. This specific community influences fertility potential significantly. Studies show that microbial diversity is crucial for maintaining a healthy uterine environment. A balanced microbiome can enhance endometrial receptivity during implantation.
Research indicates that certain bacteria are linked to improved fertilization rates. For instance, Lactobacillus species are often found in healthy endometrial samples. Their presence may support embryo development and successful pregnancy outcomes. Conversely, an imbalance in microbial populations can lead to conditions like infertility or ectopic endometrium.
Advances in Research Methods
Recent advancements have changed how scientists study the microbiome. Traditional culture-based methods often missed many microbes present in the uterus. High-throughput DNA sequencing has emerged as a powerful tool. This technology allows researchers to analyze the entire microbial community more accurately.
Using uterine cavity sampling, scientists can now collect endometrial samples efficiently. They analyze these samples to determine relative abundance and diversity of microbes. This method provides insights into how different microbial profiles affect fertility.
For example, studies have shown that certain bacterial genomes correlate with successful embryo transfer outcomes. Understanding these connections can lead to better fertility treatments and interventions.
Clinical Implications
The relationship between the endometrial microbiome and fertility has important clinical implications. Healthcare providers may begin to consider microbiome assessments in fertility evaluations. By understanding individual microbial profiles, they can tailor treatments more effectively.
This approach may involve probiotics or other interventions aimed at restoring a healthy balance of bacteria in the uterus. Such strategies could improve reproductive outcomes for couples facing infertility challenges.
Genital Tract Microbiome’s Role
Dominance of Lactobacillus
A healthy vaginal microbiome is primarily dominated by the Lactobacillus species. This bacterium helps maintain a balanced vaginal milieu. It produces lactic acid, which keeps the pH level low. A low pH is essential for inhibiting harmful bacteria. Studies show that women with a predominance of Lactobacillus have better reproductive health outcomes.
Vaginal swabs often reveal this dominance in fertile women. The presence of Lactobacillus supports vaginal homeostasis. This balance can influence fertility positively. In contrast, a decrease in these beneficial bacteria can lead to conditions like bacterial vaginosis.
Impact of Pathogens
Pathogens like Chlamydia trachomatis and Gardnerella vaginalis can severely impact fertility. Chlamydia trachomatis is known for causing inflammation in the genital tract. This inflammation can result in scarring and blockages in the fallopian tubes. Such damage may prevent successful fertilization or implantation.
Similarly, Gardnerella vaginalis is associated with bacterial vaginosis. This condition alters the normal vaginal flora. Women with bacterial vaginosis often experience difficulty conceiving. The imbalance in the cervical flora can affect sperm motility and survival.
Importance in ARTs
The genital tract microbiome plays a crucial role during assisted reproductive treatments (ARTs). Research indicates that a balanced microbiota can enhance the success rates of procedures like in vitro fertilization (IVF). A healthy endometrial microbiota supports embryo implantation.
Studies suggest that the composition of vaginal secretions impacts ART outcomes. Women with a diverse and healthy vaginal microbiota tend to respond better to treatment. They also experience fewer complications during pregnancy.
Monitoring the vaginal microbiome through vaginal samples can provide valuable insights. Regular testing allows healthcare providers to identify any imbalances early on. Addressing issues like bacterial vaginosis can improve overall fertility potential.
Gut Microbiome’s Influence on Hormones
Hormone Regulation
The gut microbiome plays a crucial role in regulating hormones. It consists of trillions of bacteria that interact with the body. These bacteria produce metabolites that can influence hormone levels. For example, lactobacillus species, including lactobacillus iners, are known to impact estrogen metabolism.
Hormones like estrogen and progesterone are vital for reproductive health. They help regulate menstrual cycles and ovulation. An imbalance in these hormones can lead to fertility issues. Studies show that women with irregular cycles often have altered gut microbiomes.
Impact on Fertility
Hormonal imbalances can significantly affect fertility. Low estrogen levels may lead to anovulation, where no eggs are released from the ovaries. This condition can make conception difficult or impossible. Furthermore, high levels of stress hormones can disrupt the reproductive system.
Research indicates that gut health influences overall hormone balance. A healthy gut microbiota can help maintain normal hormone levels. Conversely, an unhealthy microbiome may contribute to conditions like polycystic ovary syndrome (PCOS). PCOS is a common cause of infertility in women.
Pathways to Reproductive Health
Several pathways link gut microbiota to reproductive health. One pathway involves the immune system. The gut microbiome helps regulate immune responses, which can affect reproductive function. An imbalance may lead to inflammation, impacting fertility.
Another pathway is through nutrient absorption. The gut microbiome aids in breaking down food and absorbing nutrients. Essential nutrients like vitamins and minerals play a role in hormone production. A deficiency in these nutrients can lead to hormonal imbalances.
The gut-brain axis is important. This connection between the gut and brain affects stress levels and emotional well-being. High stress can disrupt hormonal balance, further influencing fertility.
Immune Function and Reproductive Health
Microbiome Influence
The microbiome plays a crucial role in shaping the immune system. It consists of trillions of microorganisms living in and on our bodies. These microbes help train the immune system to distinguish between harmful and harmless agents. A balanced microbiome can enhance immune responses, reducing the risk of infections.
Research shows that an imbalance in microbiota can lead to increased inflammation. This inflammation affects reproductive health. For example, women with altered vaginal health may experience issues related to female infertility. Conditions like bacterial vaginosis can disrupt normal flora, leading to complications during pregnancy.
Immune System Impact
Immune function significantly influences reproductive physiology. A well-functioning immune system supports healthy reproductive outcomes. It helps maintain a suitable uterine condition for embryo implantation. Women with compromised immunity may face challenges such as infectious infertility. This condition can result from chronic infections that affect the reproductive organs.
Studies indicate that women with autoimmune disorders have higher rates of infertility. The immune system mistakenly targets healthy tissues, impacting reproductive health. Furthermore, successful implantation relies on a balanced immune response. An overactive or underactive immune system can hinder this process.
Long-term Effects
The initial colonization of the newborn’s microbiome occurs at birth. Factors such as mode of delivery influence this colonization. Vaginal births expose infants to beneficial bacteria, promoting a healthier microbiome. This early exposure impacts long-term health outcomes.
A well-established microbiome contributes to optimal immune function throughout life. Research indicates that infants with diverse microbiomes may have better immune responses later on. This diversity can reduce the risk of allergies and autoimmune diseases.
In adults, an imbalanced microbiome may lead to chronic inflammation. This inflammation can affect fertility by altering hormone levels, including progesterone. Hormonal balance is essential for menstrual regularity and ovulation.
Impact of Microbiome Disorders
Dysbiosis Defined
Dysbiosis refers to an imbalance in the normal microbiota of the body. This condition can occur due to various factors. Antibiotic use is a common cause. It can disrupt healthy bacteria, allowing harmful pathogens to thrive. Poor diet also plays a role. High sugar and processed foods can alter gut flora. Stress and hormonal changes may contribute as well.
Infertility and Dysbiosis
Dysbiosis in the genital tract can significantly affect fertility. The presence of abnormal microbiota may lead to inflammation. Inflammation can damage reproductive tissues. This damage may hinder implantation or embryo development. Research shows that women with dysbiosis have higher rates of infertility. An imbalance in vaginal bacteria can create an environment unsuitable for sperm survival.
Bacterial Vaginosis and Fertility
Asymptomatic bacterial vaginosis (BV) is another concern. BV occurs when there is an overgrowth of certain bacteria in the vagina. Many women do not experience symptoms but still face risks. Studies indicate that BV is linked to fertility issues. It can create an acidic environment that affects sperm motility. This makes it harder for sperm to reach the egg.
Women with BV may also be at risk for pelvic inflammatory disease (PID). PID can lead to scarring of the fallopian tubes, further complicating conception. Understanding this connection is vital for addressing fertility challenges.
Associated Pathogens
Several associated pathogens are involved in dysbiosis-related infertility. These include Gardnerella vaginalis and Mycoplasma hominis. Both are often found in women with BV. Their presence can lead to complications during pregnancy as well.
The relationship between these pathogens and reproductive health highlights the importance of a balanced microbiome. Maintaining a healthy microbial community is crucial for overall reproductive success.
Addressing Dysbiosis for Better Fertility
Diagnostic Methods
Doctors can use several methods to diagnose dysbiosis in women. A common approach is a stool test. This test analyzes the composition of gut bacteria. It helps identify imbalances that may affect fertility.
Another method is a vaginal swab. This test checks for the presence of specific bacteria like lactobacillus jenseni and lactobacillus crispatus. These bacteria are crucial for maintaining a healthy vaginal microbiome. Abnormal levels may indicate dysbiosis, which can lead to conditions such as endometriosis or chronic endometritis.
Pelvic examinations can also reveal signs of dysbiosis. Symptoms such as pelvic discomfort may prompt further investigation. Doctors may perform imaging tests to understand any underlying issues better.
Treatment Options
Restoring a healthy microbiome balance often involves targeted treatments. Probiotics are one effective option. They introduce beneficial bacteria back into the system. Supplementation with specific strains can help combat dysbiosis.
Prebiotics also play a significant role. They provide nourishment for good bacteria, promoting their growth. Foods rich in prebiotics include garlic, onions, and bananas. Integrating these foods into the diet can support microbiome health.
In some cases, medical procedures may be necessary. Women who have undergone hysteroscopy or hysterectomy might need additional care to restore balance. Treatments for conditions like ovarian endometriosis often focus on reducing inflammation and restoring normal function.

Benefits of Probiotics and Prebiotics
The potential benefits of probiotics and prebiotics are notable in treating dysbiosis. Studies show that probiotics can improve symptoms related to endometrial fluid issues. They may enhance overall reproductive health by balancing the vaginal microbiome.
Probiotics can also reduce the risk of obstetrical problems during pregnancy. Some research suggests they may lower the chances of complications associated with dysbiosis. This includes conditions linked to chronic endometritis.
Prebiotics contribute significantly as well. They help maintain a diverse microbiome, which is vital for overall health. A balanced microbiome supports not just fertility but also general well-being.
Women facing challenges related to fertility should consider these options seriously. The relationship between microbiome health and fertility is clear. Addressing dysbiosis can lead to improved reproductive outcomes.
Nutrition and Lifestyle Changes
Diet’s Role
Diet plays a crucial role in maintaining a healthy microbiome. Healthy women often consume a variety of foods that support microbial diversity. Foods rich in fiber, such as fruits, vegetables, and whole grains, feed beneficial bacteria. These bacteria help regulate hormonal changes and improve overall health.
Studies show that diets high in processed foods can lead to dysbiosis. Dysbiosis refers to an imbalance in the microbiome. This imbalance can negatively affect fertility outcomes. A balanced diet promotes the growth of healthy communities within the gut.
Suggested Lifestyle Changes
Lifestyle changes can also enhance microbiome health and fertility. Regular physical activity is vital. Exercise helps reduce stress and supports a diverse microbiome. Aim for at least 150 minutes of moderate exercise each week.
Sleep quality is another important factor. Poor sleep affects hormonal balance and stress levels. Aim for 7-9 hours of quality sleep per night. This practice can improve both mental well-being and microbiome health.
Mindfulness practices, such as yoga or meditation, can help manage stress. Stress impacts the microbiome by altering its composition. Reducing stress supports a healthier environment for beneficial bacteria.
Impact of Stress and Environment
Stress has a significant impact on the microbiome. It can lead to hormonal changes that disrupt microbial balance. High-stress levels may contribute to conditions like anxiety and depression, which further affect fertility.
Environmental factors also play a role in shaping the microbiome. Exposure to pollutants and chemicals can harm beneficial microbes. Studies have shown that these environmental changes can influence microbial communities.
A clean environment is essential for maintaining a healthy microbiome. Using natural cleaning products reduces exposure to harmful chemicals. Limiting processed foods minimizes intake of artificial additives that may disrupt gut health.
Research shows that certain technologies help study the microbiome’s response to various conditions. Advanced methodologies allow scientists to analyze microbial communities in detail. These studies provide insight into how nutrition and lifestyle choices impact fertility.
Integrating Microbiome Health in Treatments
Microbiome Assessments
Microbiome studies show a strong link between the human microbiome and fertility. Assessing the microbial community can reveal important insights. For example, analyzing specific bacteria like Bacteroides can help understand reproductive health. This information should be integrated into fertility treatments.
Many fertility experts advocate for microbiome assessments. They believe these evaluations can lead to better treatment outcomes. Understanding an individual’s unique microbiome profile allows for tailored interventions. This approach may enhance the effectiveness of existing fertility treatments.
Personalized Treatment Plans
Personalized treatment plans based on microbiome analysis are crucial. Each person’s microbiome is different, which influences their health. Probiotics can play a role in this personalization. These beneficial bacteria can help restore balance in the microbiome.
For instance, women with specific imbalances may benefit from targeted probiotic therapies. Research indicates that correcting these imbalances can improve reproductive function. Fertility specialists should consider these factors when developing treatment plans.
Need for Further Research
Further research on microbiome-targeted therapies is essential in reproductive medicine. Current studies provide a foundation, but more data is needed. Investigating how various microbes affect fertility will lead to new insights.
Medical surgical specialties must prioritize this area of study. The connection between the microbiome and conditions like Mycobacterium tuberculosis or Burkholderia infections requires deeper exploration. Understanding these relationships can shape future treatments.
Sequencing technologies have advanced significantly. They allow researchers to analyze complex microbial communities effectively. By utilizing these tools, scientists can uncover the role of the microbiome in fertility issues.
Clinical Implications
Integrating microbiome health into clinical practice has practical implications. Fertility clinics should adopt microbiome profiling as part of standard procedures. This integration could lead to improved patient outcomes and satisfaction.
Patients often seek comprehensive solutions to their fertility challenges. Addressing the microbiome offers a novel approach that aligns with holistic care principles. It empowers patients by providing them with actionable insights into their health.
Final Remarks
Understanding the microbiome’s connection to fertility is crucial for anyone looking to enhance reproductive health. The interplay between the genital and gut microbiomes can significantly affect hormonal balance, immune function, and overall wellness. Addressing issues like dysbiosis through nutrition and lifestyle changes can pave the way for better fertility outcomes.
Take charge of your reproductive health today. Consider integrating microbiome-focused strategies into your routine. Consult with healthcare professionals to tailor a plan that suits your needs. Awareness and proactive steps can make a real difference in your fertility journey.
Frequently Asked Questions
What is the microbiome?
The microbiome is a collection of microorganisms, including bacteria, fungi, and viruses, that live in various parts of the body. It plays a crucial role in digestion, immunity, and overall health.
How does the microbiome affect fertility?
A balanced microbiome can enhance reproductive health by regulating hormones, supporting immune function, and maintaining a healthy environment for conception. Dysbiosis, or imbalance, may hinder fertility.
What is the genital tract microbiome?
The genital tract microbiome consists of microorganisms residing in the reproductive organs. A healthy genital microbiome supports vaginal health and can influence fertility outcomes.
Can gut health impact reproductive hormones?
Yes, the gut microbiome influences hormone production and regulation. A healthy gut can help balance estrogen and progesterone levels, which are essential for fertility.
What are microbiome disorders?
Microbiome disorders occur when there’s an imbalance of microorganisms in the body. This dysbiosis can lead to various health issues, including infertility.
How can I improve my microbiome for better fertility?
You can enhance your microbiome by eating a balanced diet rich in fiber, probiotics, and prebiotics. Regular exercise and stress management also contribute to a healthier microbiome.
Is there a link between nutrition and microbiome health?
Absolutely! Nutrient-rich foods support microbial diversity and function. A healthy diet fosters a balanced microbiome, which is vital for reproductive health.
